Cancer comes in many different forms, and it is not unusual for diagnosed patients to endure multiple kinds of treatments before one that is effective against their particular form of cancer is found.
If it takes too long for doctors to find the right treatment, the consequences can be fatal.
The severity of cancer has fuelled physicians and scientists from all walks of life to explore any possible solution, including those that seem natural to those that may at times seem unconventional.
Well, researchers are now taking vaccines, which typically target viruses and bacteria, and reworking them to zero in on the patient's specific cancer cells.
Physicians and scientists led by Catherine Wu at the Dana-Farber Cancer Institute in Boston just presented their results of their new cancer therapy to the American Association for Cancer Research (AACR) in Washington, DC.
Their personalised vaccines have prevented early relapse in 12 patients with skin cancer, while also boosting patient immunity when combined with a cancer drug.
While earlier cancer vaccines targeted a singular cancer protein found ubiquitously among patients, these personalised vaccines contain neoantigens, which are mutated proteins specific to an individual patient's tumour.
These neoantigens are identified once a patient's tumour is genomically sequenced, providing physicians with the information they need to pinpoint unique mutations.
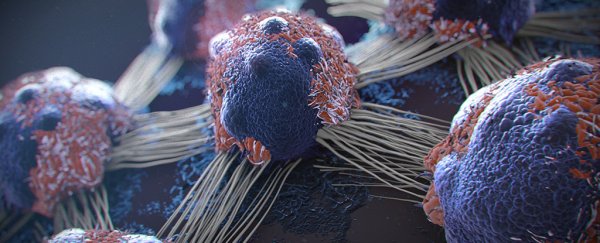
Once a patient's immune system is provided a dose of the tumour neoantigens, it can activate the patient's T cells to attack cancer cells.
Unlike previous attempts towards cancer vaccines, which did not produce conclusive evidence in halting cancer growth, Wu's team made their personal vaccine much more specific to each patient's cancer, targeting about 20 neoantigens per patient.
The vaccines were injected under the patients' skin for a period of five months and indicated no side effects and a strong T cell response.
All of Wu's patients who were administered the personal vaccine are still cancer-free more than 2.5 years after the trial.
However, some patients with an advanced forms of cancer also needed an some extra punching power to fend off their diseases.
Two of Wu's patients who did relapse were administered an immunotherapy drug, PD-1 checkpoint inhibitor, in addition to the personalised vaccine.
Working in conjunction with the enhanced T cell response from the vaccine, the drug makes it difficult for the tumour to evade the immune cells. The fusion of the two therapies eliminated the new tumours from both patients.
But we can't get too excited yet. While these results are promising, the therapies are relatively new and require much more clinical testing.
Many physicians around the world are working together to test the potency of neoantigens in order to verify if the vaccine works better than current immunotherapy drugs over a sustainable period of time.
Personalised vaccines are costly and take months to create, a limiting factor in providing care to patients with progressing cancers.
Still, this study is an encouraging sign for many oncologists who are interested in using the immune system to fight cancer.
More than a million new patients are diagnosed with cancer each year in the U.S. alone, and even in situations where the cancer is treatable, the available chemotherapy agents themselves can be very toxic.
If proven safe and effective, this personalised cancer vaccine could give patients around the world hope for powerful treatment with fewer side effects.
This article was originally published by Futurism. Read the original article.