Scientists in the US have discovered a new class of antibiotic that has been shown to kill Staph and Strep throat infections in mice. They say the way it kills bacteria will make it very difficult for them to evolve resistance in response to the attacks.
Last month, a report chaired by US economist Jim O'Neill predicted that 300 million people will die prematurely by the year 2050 thanks to antimicrobial resistance, if nothing is done to solve the problem. The report went on to add that our global GDP would dip by 0.5 percent by 2020 and will end up 1.4 percent smaller by 2030, purely due to the steady march of resistant bacteria.
In 2013, the chief medical officer of the UK, Sally Davies, announced that antimicrobial resistance would be put on the government's national risk register of civil emergencies, to join the equally serious threats of terrorism, the pandemic flu, and major flooding.
Antimicrobial resistance is a huge problem, but we might finally have the upper hand in this power struggle between man and bug - a new antibiotic called teixobactin, which has been shown to kill a wide range of drug-resistant bacteria in lab mice, including those responsible for tuberculosis and septicaemia, plus Clostridium difficile colitis (C. dif) - the most common gut bug infection.
"Teixobactin kills exceptionally well. It has the ability to rapidly clear infections," lead researcher and director of the Antimicrobial Discovery Centre at Northeastern University, Kim Lewis, told Ian Sample at The Guardian.
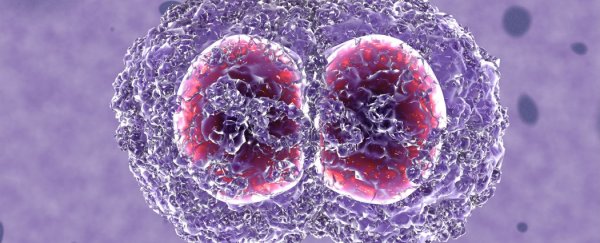
The secret to Teixobactin's success is that it prevents microbes from being able to construct their cell walls, and holes in your cell walls means certain death. In fact, the antibiotic ended up killing 100 percent of the bacteria it came into contact with, and no survivors means there's no one to evolve resistance. "That's an Achilles' heel for antibiotic attack," the researcher who discovered this ability, Tanja Schneider from the University of Bonn, told Sample. "It would take so much energy for the cell to modify this, I think it's unlikely resistance will appear this way."
As Kelly Servick explains at Science Magazine, resistance usually occurs when a fraction of a population of microbes somehow survives an antibiotic attack because of a particular mutation, and then those mutated bacteria multiply into a separate resistant population.
"My guess is that if resistance is going to develop against Teixobactin, it will take more than 30 years for that to occur," Lewis told CBS News.
Not only did Teixobactin kill off 100 percent of the bacteria it came into contact with, including Staphylococcus aureus (Staph infection) and Streptococcus pneumoniae (Strep throat), but it cleared these infections without any side-effects.
Which is all great, but perhaps even more exciting is how the antibiotic was discovered. "Most antibiotics are isolated from bacteria or fungi that churn out lethal compounds to keep other microbes at bay," says Sample at The Guardian. "But scientists have checked only a tiny fraction of bugs for their ability to produce potential antibiotics because 99 percent cannot be grown in laboratories."
Since the first antibiotic, Penicillin, was discovered by accident in 1928 by Alexander Fleming, scientists haven't had a particularly efficient way of finding more. But recently, Kim Lewis's team developed a device they're calling the iChip, which can culture bacteria in their natural habitat - in this case, dirt. Bacteria are inserted into the device between two permeable sheets and dug into the ground, where the bacteria are free to grow into colonies as they would in the wild, except for the fact that they're confined to their iChip chambers.
After two weeks, the researchers retrieved their iChip and were able to test the colonies that had grown in their natural habitat. "To do this, they covered the top of the iChip with layers of pathogens," says Sample. "Bugs that produced natural antibiotics revealed themselves by killing the pathogens above them."
The team paired up with NovoBiotic, a Massachusetts-based pharmaceuticals start-up, and researchers at the University of Bonn, and screened 10,000 different types of soil bacteria - cultured in the iChip - for antibiotics. They found 25 new antibiotic compounds, teixobactin being the most high-achieving of the lot. They published their results in Nature today.
Servick reports at Science Magazine that Teixobactin was so effective, it also outperformed Vancomycin - the antibiotic we currently rely on to treat methicillin-resistant Staphylococcus aureus (MRSA) - by a factor of 100. "In mice infected with MRSA, injections of teixobactin led to a 100 percent survival rate at lower doses than vancomycin," she says.
It's exciting stuff, but it's still going to be a while before people can be treated with the antibiotic. Human trials are set to begin in about two years, and if they go well, development for the market will follow.
"Another shortcoming of Teixobactin is that it only works against bacteria that lack outer cell walls, known as Gram-positive bacteria, such as MRSA, Streptococcus and TB," says Sample at The Guardian. "It doesn't work against Gram-negative bacteria, which include some of the most worrying antibiotic-resistant pathogens, such as Klebsiella, E. coli and Pseudomonas."
But hopefully that's something Lewis's team's new iChip method will help solve.
As Mark Woolhouse, professor of infectious disease epidemiology from the University of Edinburgh in the UK, told Sarah Knapton at The Telegraph:
"Any report of a new antibiotic is auspicious, but what most excites me about the paper is the tantalising prospect that this discovery is just the tip of the iceberg. Most antibiotics are natural products derived from microbes in the soil. The ones we have discovered so far come from a tiny subset of the rich diversity of microbes that live there.
Lewis et al. have found a way to look for antibiotics in other kinds of microbe, part of the so-called microbial ' dark matter' that is very difficult to study."
Sources: The Guardian, Science Magazine, The Telegraph