Capsules of fat just over a hundred nanometres in size could be used to discreetly sneak drugs across one of the body's toughest border crossings, to specifically target glioblastoma - a seriously aggressive type of brain cancer.
So far the research has only proven itself in mice, but if all goes well, it could provide a much-needed treatment for tumours that typically claim a patient's life within just 15 months of diagnosis.
MIT researchers have designed a type of nanoparticle that can effectively move from the patient's blood into the brain tissue while carrying a dual payload of chemicals for attacking the tumour.
Getting anything into the brain via the bloodstream is complicated by a wall of tightly interconnecting cells that stands in the way. This blood-brain barrier is usually a good thing, as it prevents bacteria and viruses from getting into your grey matter, causing havoc with your most vital organ.
Unfortunately this neurological Great Wall also makes it a lot harder to get unfamiliar chunky molecules into the brain - such as the types of toxins we might want to use to attack particularly nasty cancers.
Glioblastoma multiforme (GBM) is about as bad as tumours come; it's a common form of brain cancer that starts off as a type of support cell called an astrocyte. The tumours are so aggressive, if you're unfortunate enough to get one you've got a five percent chance of still being around in five years.
The good news is that we have ways to kill them: the chemotherapy drug temozolomide methylates the DNA of tumour cells, triggering their death. Then, to make sure the cancer cells don't simply fix the damage, a second type of drug called a bromodomain inhibitor can be administered to sabotage the repair mechanisms.
But, as we already mentioned, the blood-brain barrier gets in the way - it does too good a job screening such drug molecules. On top of that, the actions of these toxins don't necessarily limit themselves to tumour cells.
To get around both problems, the MIT scientists designed drug-runners that could slip through the boundary and target the tumour.
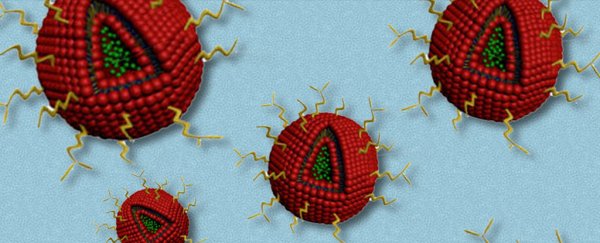
The nanoparticles are lipid capsules with a bromodomain inhibitor embedded in their shell, and a temozolomide in their centre.
By coating the whole thing in a type of iron-binding protein called a transferrin along with a 'stealthy' chemical called polyethylene glycol, the 140-nanometre-wide particles could make use of unique receptors in the blood-brain barrier that give them a pass.
Once on the other side, those transferrin molecules could stick to similar receptors used by the tumour, bypassing healthy brain tissue.
Cancerous mice given daily doses of the particles survived up to twice as long as mice that received no treatment. They also showed less non-cancer tissue damage from the drugs, compared with mice that received treatment in a conventional form.
Since the nanoparticle components are already FDA approved, the road to testing on humans should be a relatively smooth one.
"Our goal was to have something that could be easily translatable, by using simple, already approved synthetic components in the liposome," says the report's lead author Fred Lam from MIT's Koch Institute for Integrative Cancer Research.
"This was really a proof-of-concept study [showing] that we can deliver novel combination therapies using a targeted nanoparticle system across the blood-brain barrier."
Other studies have suggested using viruses or even genetically modified bacteria to overcome similar hurdles in reaching and destroying glioblastoma cells.
Big, bold ideas are clearly needed to search and destroy a big, bad form of cancer. And we can hope that one of them will prove useful in the coming years.
This research was published in Scientific Reports.