It's no secret that depression meds don't always work, and a recent study by scientists in Japan gives us a new framework for understanding why.
Depression – aka major depressive disorder (MDD) – affects an estimated 300 million people across the globe, but despite the enormous scale of the disease, there's still a huge amount we don't know about what causes it.
In terms of treatment, one of the most glaring issues is that the most common form of antidepressants – selective serotonin reuptake inhibitors (SSRIs) – are ineffective for an estimated 30 percent of patients.
Now, new research could get us closer to understanding why this is, in addition to helping us diagnose and treat the condition with greater accuracy.
"It has always been speculated that different types of depression exist, and they influence the effectiveness of the drug," says computational neuroscientist Kenji Doya from the Okinawa Institute of Science and Technology Graduate University.
"But there has been no consensus."
Customarily, depression is diagnosed by clinical assessment carried out by medical practitioners, but because this isn't exactly a perfect science, in recent years researchers have increasingly sought to find potential biomarkers for depression.
One of the ways of doing this is by studying brain activity, monitoring functional magnetic resonance imaging (fMRI) signals.
In the new study, to find a way to analyse and categorise potentially different sub-types of depression, Doya and his team performed a cluster analysis (a data-driven grouping exercise) on a range of health data supplied by 134 people.
Half of the participants had depression, while the other half were people with no history of the condition, who acted as controls.
From this group, the researchers obtained fMRI data, gene expression information, and responses to clinical questionnaires about their sleep patterns, mental health conditions, and other aspects of their life history.
With all the data in hand, the researchers ran their cluster analysis, looking for discrete forms of relationships that could indicate meaningful subtypes of depression from over 3,000 measurable features recorded in the data set – a kind of analysis the team says has never been done.
 (Neural Computational Unit/OIST)
(Neural Computational Unit/OIST)
"The major challenge in this study was to develop a statistical tool that could extract relevant information for clustering similar subjects together," explains first author of the study, statistician Tomoki Tokuda.
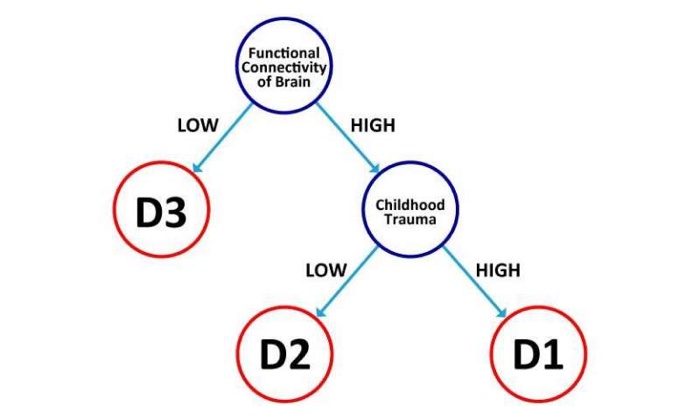
Using a specialised analytical tool for investigating high-dimensional data containing heterogeneous types of features that the team developed last year, the researchers identified different sub-types of depression, called D1, D2, and D3.
According to the results, individuals with the D1 sub-type are characterised by high functional connectivity of the brain and a history of childhood trauma.
In contrast, the D2 participants exhibited high functional connectivity of the brain, but had no history of childhood trauma.
Finally, people with the D3 sub-type reflected low functional connectivity of the brain and had not experienced childhood trauma.
The cluster analysis also revealed that SSRIs are likely to be effective for people with the D2 and D3 sub-types of depression, but D1s – those with high functional connectivity between the brain's different regions and experience of childhood trauma – would find the drugs ineffective.
The researchers acknowledge it will take further, larger studies with much greater numbers of participants to back up these findings, but the methodology they've come up with could offer a powerful new guide to help health researchers understand the complexity of depression – and where individual patients fit in to the mix.
"This is the first study to identify depression sub-types from life history and MRI data," Doya explains.
"It provides scientists studying neurobiological aspects of depression a promising direction in which to pursue their research."
The findings are reported in Scientific Reports.
