Even the most exciting breakthrough medical treatment can be rendered obsolete by a particularly insurmountable obstacle: time.
If a treatment only works temporarily, it has little chance of making a significant difference in the lives of patients, which is why the latest news from the University of Miami's Diabetes Research Institute is so exciting.
A year after transplanting insulin-producing islet cells into the omentum of a woman with a particularly unwieldy form of type 1 diabetes, the cells continue to operate as hoped.
She no longer needs to receive insulin via injections or an insulin pump and is in good health.
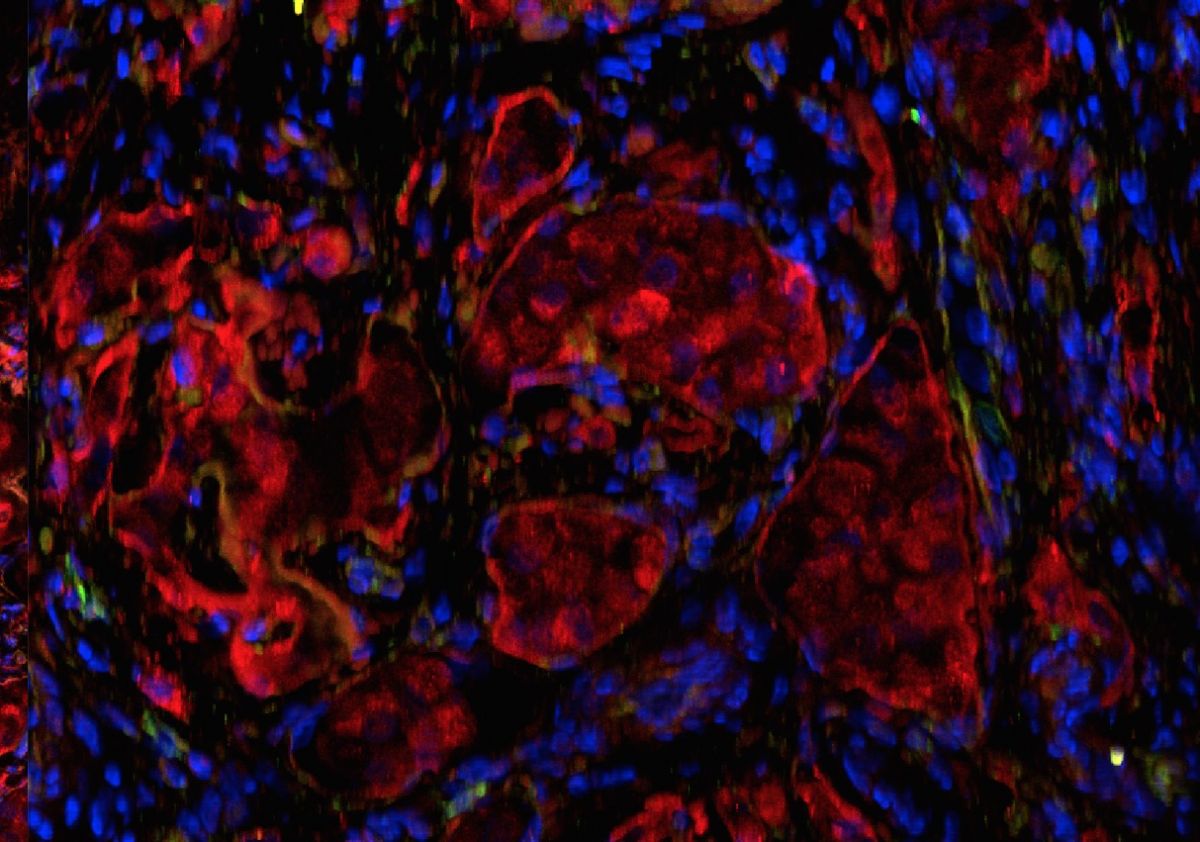 Fluorescence microscopy of islets in the omentum transplanted within the biologic scaffold. In red (insulin staining) and blue (DAPI nuclear staining). Credit: Diabetes Research Institute/University of Miami Miller School of Medicine
Fluorescence microscopy of islets in the omentum transplanted within the biologic scaffold. In red (insulin staining) and blue (DAPI nuclear staining). Credit: Diabetes Research Institute/University of Miami Miller School of Medicine
By using the omentum, a fatty membrane in the belly, as the transplant site, the researchers were able to avoid complications associated with the traditionally used site, the liver.
The longterm goal of the research is to identify a suitable location for a pancreas-mimicking mini-organ called the BioHub.
Based on this patient's response, the omentum is looking like it just may be the ideal spot.
Prior to this transplant, the patient's entire life revolved around her diabetes.
"Her quality of life was severely impacted. She had to move in with her parents. And, if she traveled, she had to travel with her father," the study's lead author, David Baidal, told HealthDay.

Unfortunately, she's not alone in having diabetes control her life. According to the US Centres for Disease Control, 9.3 percent of the United States population has diabetes, and 28.7 percent of those people have to inject insulin to manage their disease.
If improperly treated, diabetes can lead to a range of ailments, from blindness and high blood pressure to nerve damage or even death.
This patient's positive reaction to her islet cells transplant could be the first step to helping those millions of people live normal, healthy lives free from the burden of constantly managing their disease.
"We're exploring a way to optimise islet cell therapy to a larger population," said Baidal. "This study gives us hope for a different transplant approach."
This article was originally published by Futurism. Read the original article.