A link between inhibiting brain inflammation and slowing the onset of Alzheimer's has been identifed in mice, and scientists say the discovery could pave the way for the development of new treatments and preventative measures for the disease.
By blocking a particular receptor in the brains of mice, a team from Southampton University was able to prevent some of the associated memory and behaviour problems associated with Alzheimer's. "These findings are as close to evidence as we can get to show that this particular pathway is active in the development of Alzheimer's disease," said lead researcher, Diego Gomez-Nicola. "The next step is to work closely with our partners in industry to find a safe and suitable drug that can be tested to see if it works in humans."
The link between brain inflammation and Alzheimer's is well-established, but there's a growing body of evidence that suggests this inflammation could be the cause of the disorder rather than the result of it. Theoretically, that means if the inflammation can be stopped, so can Alzheimer's - or at least some of the effects of it.
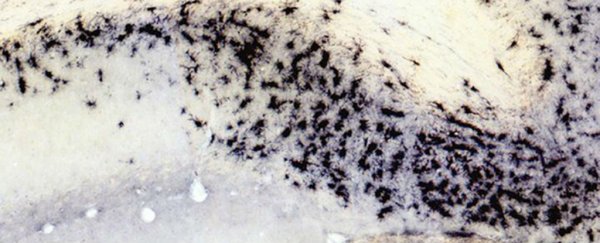
The researchers first compared tissue samples from healthy human brains to those from patients diagnosed with Alzheimer's. They found more of the immune cells called microglia in the Alzheimer's-affected brains, with the severity of the disease correlating with the activity of the molecules regulating the numbers of microglia.
Those findings then informed the second part of the research: looking for microglia in mice that had been bred to develop features of the Alzheimer's condition. By blocking the receptor responsible for regulating the immune cells, a receptor known as CSF1R, microglia numbers remained steady. What's more, the inhibitor prevented the loss of communication points between the nerve cells.
It's a big jump from lab mice to human beings, but the findings open up a promising new lead for those working on a cure for Alzheimer's. "While this basic science research provides strong evidence, the challenge will now be to develop medicines for people with dementia," Mark Dallas, a neuroscientist at Reading University who was not involved in the research, told Ian Sample at The Guardian.
"Too often, this has been the stumbling block in turning observations in the laboratory into a workable therapy. Excitingly, it does however highlight new avenues for researchers to exploit and strengthens the case for targeting other cell types within the brain in the fight against Alzheimer's."
While microglia were kept at a healthy level and brain nerve cell connections were maintained in the treated group of mice, the treatment did not stop the build-up of amyloid plaques in the brain - another condition associated with the spread of Alzheimer's. The good news is that CSFR1-inhibiting drugs are already in use for other applications, which may speed up the development and approval process for an Alzheimer's treatment.
The new study has been published in the journal Brain.