Researchers in the US have been testing a new type of antidepressant medication on rats, and say it's able to treat the symptoms of depression in less than a day, compared to the three to eight weeks it takes current drugs to work. If the results can be replicated in humans, the drug could offer a much more effective option than treatments such as Prozac and Lexapro, which are only effective in only a third of patients who have been diagnosed with depression.
"Our results open up a whole new class of potential antidepressant medications," lead researcher Scott Thompson from the University of Maryland said in press release. "We have evidence that these compounds can relieve the devastating symptoms of depression in less than one day, and can do so in a way that limits some of the key disadvantages of current approaches."
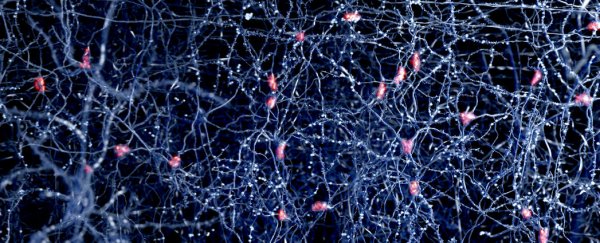
Currently available antidepressant medications such as Prozac and Lexapro work by increasing the levels of the neurotransmitter serotonin in the brain. Known as selective serotonin reuptake inhibitors - or SSRIs - they are believed to work by limiting the reabsorption of serotonin into the brain's presynaptic cell, and this readjustment of serotonin levels appears to help the brain cells send and receive chemical messages more effectively, which can boost a person's mood.
There are a range of SSRIs that are currently available to people with depression, but each one has a different chemical make-up, so will affect a patient in a slightly different way, and could cause a range of negative side effects such as nausea, dizziness, reduced sexual desire or erectile dysfunction, drowsiness, insomnia, and weight gain. Patients will also have to wait for one or two months for these medications to relieve their symptoms, which can not only be emotionally excruciating for them, but incredibly dangerous if they happen to be suicidal.
And all of that is assuming these drugs work for the patient at all. According to a recent study:
"The rate of treatment response following first-line treatment with SSRIs is moderate, varying from 40 to 60 percent; remission rates vary from 30 to 45 percent. Up to one third of persons taking antidepressant medications will develop recurrent symptoms of depression while on therapy."
To produce a more effective medication, instead of looking into mitigating the levels of serotonin in the brain, Thompson and his team focused a different neurotransmitter - a inhibitory compound called GABA.
There are two types of neurotransmitters that communicate information around our brain - excitatory and inhibitory neurotransmitters. While excitatory neurotransmitters are responsible for stimulating the brain, inhibitory neurotransmitters are there to calm it down and balance your mood. But in people with depression, the researchers hypothesise, the excitatory messages in certain brain regions are not strong enough, and the most effective way to fight this could be to reduce the levels of inhibitory neurotransmitters in these areas.
Thompson and his team looked into a class of compounds - called GABA-NAM - that reduce the inhibitory messages that are sent via the GABA neurotransmitter. When tested in rats with depressive symptoms, not only did these compounds balance out the work of the different types of neuotransmitters to stabilise their mood in less than 24 hours, but they also minimised unwanted side effects, being able to affect only in the regions of the brain that are essential for mood regulation.
"These compounds produced the most dramatic effects in animal studies that we could have hoped for," said Thompson. "It will now be tremendously exciting to find out whether they produce similar effects in depressed patients. If these compounds can quickly provide relief of the symptoms of human depression, such as suicidal thinking, it could revolutionise the way patients are treated."
The next step will be to get the compounds ready for human trials to see if these promising results can be replicated. One thing's for sure, people with depression are in serious need of better treatments than they're currently getting, so hopefully the team is on the right track.
The results were published in the journal Neuropsychopharmacology.