In what could be compared to finding patient zero in an outbreak, researchers have traced genes for antibiotic resistance back to their source.
With an increasing variety of pathogenic bacteria evolving to protect themselves against our best chemical weapons, finding the origins of their key defences against antibiotics has become a priority.
New research from The Novo Nordisk Foundation Centre for Biosustainability in Denmark has for the first time provided evidence to back up what biologists have long suspected – the resistance genes come from the same source as the antibiotics themselves.
Antibiotics come in a rich variety of forms, but all basically do the same kind of thing – they're chemicals that interfere with mechanisms specific to the growth and maintenance of bacterial cells.
Most originated as some form of microbial weapon against other microbes, a way of clearing the environment of competitors. In fact, more than 75 percent of antibiotics we use today come from a phylum of gram-positive bacteria called Actinobacteria.
As far back as 1973, scientists noticed that there's a striking resemblance between the actions of an antibiotic-breaking enzyme found in other forms of bacteria referred to as gram-negatives and a similar group of enzymes found in Actinobacteria.
The fact that the poisoner also cooks up the antidote makes a lot of sense, but evidence for these gram-positives being the source of resistance genes was thin on the ground.
The question is; just where did these resistance genes come from in the first place?
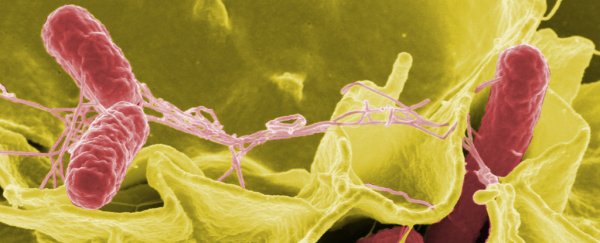
In most cases, genes for such resistance don't evolve in the superbug itself. They're stolen from another species in what's called horizontal gene transfer.
Sometimes bacterial cells in the same vicinity can swap genetic material, typically in the form of circular loops of DNA called plasmids. This can be done by either sucking up fragments of DNA that have been left behind in the environment, having a virus carry it across, or transferred through a straw-like structure called a pilus in what's called conjugation.
With the discovery of similarities in anti-antibiotic processes between the gram-negatives and Actinobacteria, researchers proposed the "producer hypothesis", suggesting the phylum was the creator of many, if not most resistance genes.
So the researchers took a closer look at a number of the resistance genes in disease-causing bacteria and found similarities, with some genes being identical between the two groups.
"It has been suspected that pathogens can obtain resistance genes from Actinobacteria for half a century. So now with the 100 percent identical genes we find the smoking gun," said researcher Xinglin Jiang.
On the face of it, gram-negative and gram-positive bacteria are so different, it's hard to imagine how genes could jump from one to the other.
While there are clear similarities between the genes, there are also enough differences to make it hard to distinguish whether the genes behind these proteins were swapped between species in an act of horizontal gene transfer, or if they evolved through some other means.
Analysing the DNA sequences surrounding the genes for the enzymes, the researchers suggested the genetic swapping could be performed through a modified form of conjugation.
The team called the process the "carry-back model", in which the pathogenic bacteria uses its pilus to inject a sequence of DNA into a nearby Actinobacteria, where it recombines with the bacteria's genome, inserting the resistance gene into the middle of the sequence.
Once the Actinobacteria cell dies, its genetic material spills into the environment, where another member of the pathogenic species can absorb it and use it.
Imagine putting an empty envelope into somebody's mail-slot. They pop a letter into it, and then you just wait until their house falls down so you can find the envelope again containing their letter.
Finding the origins of these resistance genes could prove a big win in the war against superbugs.
"We can't stop this gene transfer, but when you know which resistance genes pathogens may harbour, you can personalize the antibiotic treatment," said researcher Tilmann Weber.
"Also, with this knowledge you can try to develop new antibiotics with other properties that the pathogens don't have a defence against."
There is still a lot of research to be done on how the transferred genes interact with their new host, and how they continue to evolve together.
Knowing how the genes jump from 'patient zero', though, is a good start to fighting back against the resistance.
This research was published in Nature Communications.