A DNA vaccine that aims to prevent the Ebola virus has been tested in humans in the US and Uganda, alongside a DNA vaccine for the closely related Marburg virus - and both have been proved to be safe.
The purpose of these phase 1 trials wasn't to show how effective the vaccines were, but the results, published in The Lancet, suggest that the vaccines triggered similar immune responses in the Ugandan and American populations - a good sign, seeing as other vaccines haven't appeared as effective in African populations.
"This is the first study to show comparable safety and immune response of an experimental Ebola vaccine in an African population," said lead author Julie Ledgerwood from the US's National Institutes of Allergy and Infectious Diseases in a press release. "This is particularly encouraging because those at greatest risk of Ebola live primarily in Africa, and diminished vaccine protection in African populations has been seen for other diseases."
With the World Health Organisation recently announcing that the death toll from the Ebola outbreak, which started in a village called Guéckédou in southeastern Guinea at the end of 2013, has risen to 7,693, it's a timely development. While potential cures rapidly developed during the outbreak, vaccine development is necessarily slower.
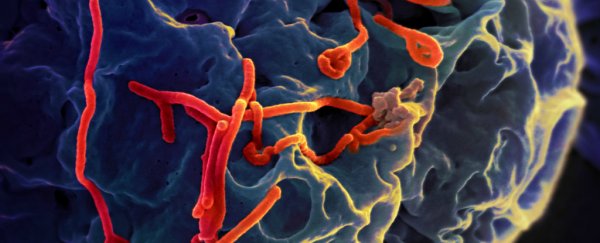
These newly-tested vaccines contain the DNA for proteins that are present on either the outer surface of the Ebola virus or certain strains of the Marburg virus - both of which are members of the Filovirus family.
This means that the vaccines effectively prime the immune system to respond when it detects these proteins, and the vaccines have already been shown to prevent the viruses in non-human primates.
In this first human trial, which took place between 2009 and 2010, scientists from the non-profit Makerere University Walter Reed Program in Uganda tested 108 healthy adults, aged between 18 and 50, from the country's capital, Kampala.
During the trials, 30 volunteers were given the Ebola vaccine, 30 were given the Marburg vaccine, 30 were given both vaccines at once, and 18 were given a placebo. The volunteers were injected at the start of the study, and then again after four and eight weeks.
The vaccines were both deemed safe whether given together or individually, and only one serious adverse reaction of low white blood cell count was recorded in a patient who had received the Marburg vaccine, but it's believed this was not related to the vaccine.
And promisingly, both vaccines triggered an immune response against the virus proteins.
Four weeks after the third dose of the Ebola vaccine had been given, just over half the volunteers had an antibody response to the Ebola Zaire protein (the strain of the virus responsibel for the current outbreak), which means their bodies were ready to fight off infection. Fourteen of the 30 patients who'd received both vaccines also had the same antibody response against Ebola Zaire.
Unfortunately, however, within 11 months of vaccination the immune response was gone, which suggests the vaccine isn't very long-lasting. The team is now using the results to look into developing an even more powerful vaccine.
"These findings have already formed the basis of a more potent vaccine, delivered using a harmless chimpanzee cold virus, which is undergoing trials in the USA, UK, Mali, and Uganda in response to the ongoing Ebola virus outbreak," said Ledgerwood in the release.
In a comment piece published in the same issue of The Lancet, Saranya Sridhar from the Jenner Institute at the University of Oxford in the UK, who wasn't involved in the research, explained that the study will hopefully help to speed up the development of a functional Ebola vaccine.
"This study is the first step on the aspirational road towards the deployment of filovirus vaccines in Africa and must serve to shake the metaphorical cobwebs that can stall our advance towards this destination," she wrote.
Source: ScienceDaily, Discovery News