In cases of a condition called jaundice, a compound called bilirubin turns a person's skin and eyes yellow. It's usually a sign that something has gone terribly wrong with the liver.
But while jaundice has widely been considered damaging to the body in itself, causing brain damage in high concentrations, a new study suggests that this bilirubin build-up can have a protective role, at least in people with malaria.
"Bilirubin was once considered to be a waste product," says Johns Hopkins molecular biologist Bindu Paul. "This study affirms that it could be one critical protective measure against infectious disease, and potentially neurodegenerative diseases."
Each year, more than 260 million residents of the tropics and subtropics are infected with malaria. This occurs when a feeding Anopheles mosquito injects saliva into their blood, and with it, the protozoan parasite Plasmodium falciparum. Around 600,000 people die from the disease each year.

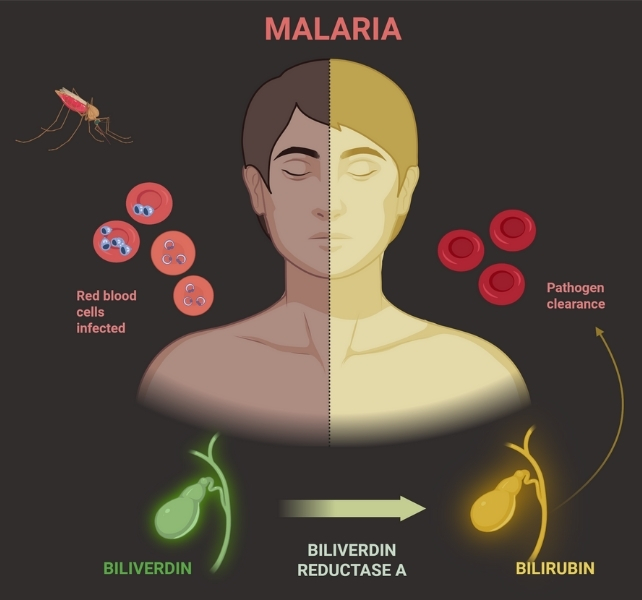
The parasite invades red blood cells where it replicates, eventually bursting the cell and releasing its supply of iron-rich heme. Toxic in high concentrations, the build-up of iron can directly affect the disease severity.
A chemical reaction that produces bilirubin, the team found, offers protection against that damage.
In some people, jaundice accompanies malaria infection, and until now it was unclear whether the compound improved or worsened patients' conditions.
In the bloodstream, bilirubin is unconjugated, meaning it can bind with other things. The liver conjugates the bilirubin, packaging it up to be excreted in our urine.
The team tested pre-liver bilirubin, the unconjugated type, in blood samples from a group of 42 volunteers infected with P. falciparum, some of whom were showing symptoms.
The asymptomatic participants had, on average, 10 times more unconjugated bilirubin in their blood plasma than their symptomatic peers, which further suggests the pigment could be protecting them from the onslaught of P. falciparum.
A series of mouse experiments provided a more detailed view of this phenomenon. When infected with a rodent-specific form of malaria, mice that were genetically engineered to lack bilirubin were easy prey to the parasite, which spread vigorously and left no survivors. Meanwhile, in the blood plasma of normal mice infected with the same disease, bilirubin levels rose and all mice survived.
Its effects on the parasite seem to occur within the infected red blood cells, where it accumulates and inhibits the growth and survival of P. falciparum by disrupting the organelles involved in food digestion and metabolism.
Bilirubin production, and the inhibition of its conjugation in the face of Plasmodium infection, "is an evolutionarily conserved resistance mechanism against malaria," the team concluded.
"Presumably, this metabolism-based defense strategy has a major evolutionary trade-off, namely, the insidious incidence of neonatal jaundice, which can potentially damage neurons in the brain."
Paul and team hope that doctors might be able to harness this natural defence strategy to reduce the heavy burden malaria imposes on humans across the world.
The research was published in Science.
