A rare genetic mutation appears to make people basically invulnerable to viruses – and it could potentially be harnessed as a therapy. Researchers have now shown this surprising viral protection can be replicated in mice and hamsters.
"We have yet to find a virus that can break through the therapy's defenses [in cell culture tests]," explains Columbia University immunologist Dusan Bogunovic, who first discovered this unusual antiviral superpower 13 years ago.
The mutation, a deficiency in interferon-stimulated gene 15 (ISG15), causes a mild yet persistent inflammation across the body. Examining patients' immune cells revealed they'd had the usual run of encounters with flu, measles, chickenpox, and mumps, yet they'd never reported feeling particularly ill as a result.
Related: Which Infectious Disease Could Be The Biggest Problem in 2025? An Expert Explains
Further investigation revealed their body's virus-fighting proteins were constantly on a low level alert, never really put away for later like in most people.
"In the back of my mind, I kept thinking that if we could produce this type of light immune activation in other people, we could protect them from just about any virus," says Bogunovic.
Now, Bogunovic and colleagues have used technology similar to mRNA vaccines to provide a temporary ISG15 deficiency in lab animals. The therapy provides instructions that help target cells build 10 proteins that the team identified as primarily responsible for the antiviral effects.
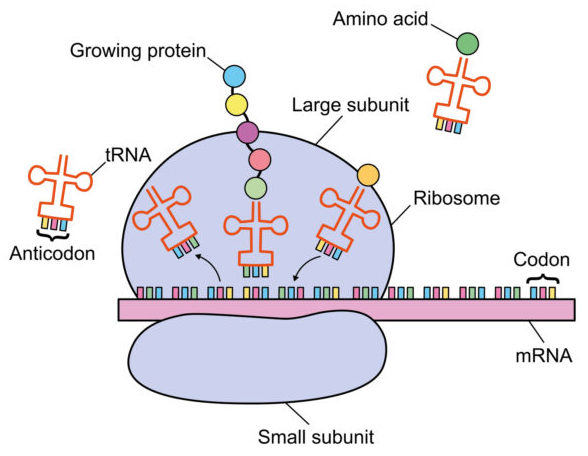
Sure enough, the bodies of test mice and hamsters successfully created more of these proteins, which attack the viruses at multiple stages of their life cycle.
The researchers then challenged the vaccinated animals with SARS-CoV-2. The protective proteins restricted the infection, but did not appear to interfere with the rest of the animals' immune systems.
"We only generate a small amount of these 10 proteins, for a very short time, and that leads to much less inflammation than what we see in ISG15-deficient individuals," explains Bogunovic. "But that inflammation is enough to prevent [viral] diseases."
The effects of inoculation were temporary, lasting up to four days. That might not sound like long enough to be very useful as a vaccine platform, but it could be administered as short-term protection for healthcare workers, even before vaccines targeting specific viruses have been developed.
"We believe the technology will work even if we don't know the identity of the virus," says Bogunovic.
This technique has the potential to massively boost our responses during future pandemics that may be similar to COVID-19 and the Spanish Flu, which have killed millions of people at a time.
However, it is still in the extremely early stages of testing. There are many challenges to resolve around how to safely deliver the mRNA to where it's needed in humans.
"Once the therapy reaches our cells, it works, but the delivery of any nucleic acid, DNA or RNA, into the part of the body you want to protect is currently the biggest challenge in the field," qualifies Bogunovic.
Recent political and social pushback against mRNA technology may also prove to be a large hurdle. But given the potential of the new method, it may be well worth the challenge.
This research was published in Science Translational Medicine.