A team of researchers from Florida International University (FIU) examined a brain protein previously associated with brain inflammation in Alzheimer's patients, in an effort to gain a deeper understanding of the relationship between the protein and the disease.
What they discovered could translate into an early signal of neurodegeneration that could eventually lead to dementia.
In mice models of Alzheimer's, elevated levels of translocator protein 18 kDa, or TSPO, were found in animals as young as six weeks, which is the equivalent of about 18-20 human years. The increase was found in the subiculum, a part of the brain crucial for memory.
Related: Learning One Word Could Help Prevent a Third of Alzheimer's Cases
The team found a similar TSPO pattern in human brain tissue taken postmortem from nine people in Colombia with a genetic mutation that causes them to develop Alzheimer's disease relatively early, typically in their 30s or 40s.
"Neuroinflammation is a very early event in Alzheimer's that influences its onset," says neuroscientist Tomás Guilarte, from FIU.
"If we can use TSPO to detect it early, right at the beginning stages of the disease, it could mean slowing progression or delaying symptoms by five or six years. That's five or six years where someone has a better quality of life."
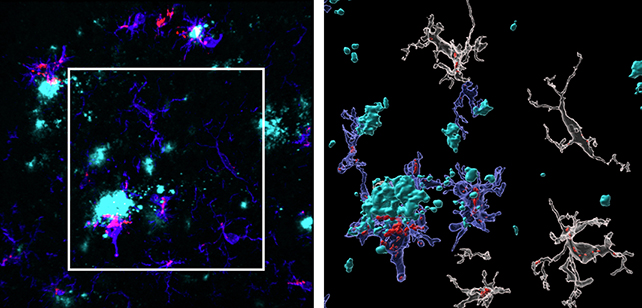
The researchers found higher levels of TSPO in female mice, mirroring data that shows women are more likely to develop Alzheimer's. They also observed an increase in TSPO coinciding with the emergence of amyloid-beta plaques – protein clumps strongly associated with the disease.
What's more, the boost in TSPO was almost entirely in the form of immune cells called microglia that were in contact with the plaques, which had both increased in number and produced more TSPO in response to the plaque build-up.
The observations provide vital insights into the origins of Alzheimer's, providing clues on the kinds of chemical reactions that might be used to slow or even stop its progress.
"We didn't see any TSPO increase in the other glial cells, like the astrocytes, which reveals the microglia are driving the majority of the inflammatory response," says Guilarte. "What we believe is happening is something goes wrong with the microglia."
"They stop doing their job in removing the plaques and just keep sending out TSPO signals. This constant signal of neuroinflammation is like adding wood to a fire."
It's important to note that this study focused on early onset, genetic cases of Alzheimer's, which are in the minority overall. However, the researchers are already working on ways to expand on this study to further pinpoint the role of TSPO.
As with many aspects of Alzheimer's, it can be difficult to untangle the causes from the consequences, but this brain biomarker may be a big help in getting a clearer picture – and ultimately, perhaps, giving us a vital early alarm bell.
"One of the biggest problems with Alzheimer's is people see it as a disease of aging, and that impacts when people get diagnosed," says neuroscientist Daniel Martinez-Perez, from FIU. "My hope is we can be part of helping people before they are too sick."
The research has been published in Acta Neuropathologica.