Higher concentrations of a specific protein in urine may be a predictor for developing dementia, based on a large, recently published study by researchers from the Netherlands and Sweden.
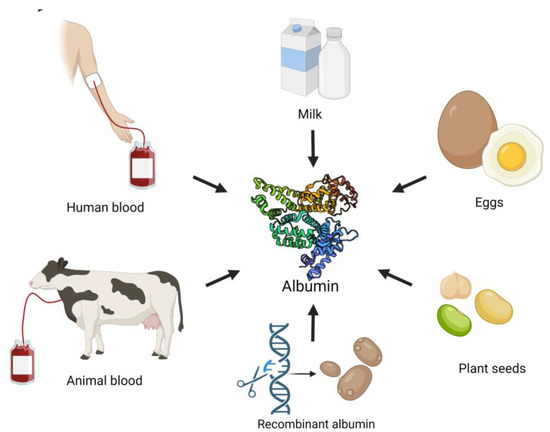
Albumin is the most abundant protein in human plasma, the liquid portion of blood. It is also a common dietary protein found in eggs, dairy products, and plant seeds.
The kidneys, which filter waste from the body, do not usually allow albumin to leak into urine. So high albumin content in urine, a condition called albuminuria, is a sign of kidney damage.
More surprisingly, it may also predict dementia risk.
Related: Chronic Insomnia May Spark Changes in The Brain That Trigger Dementia
This revelation comes courtesy of a study that included nearly 133,000 participants in Stockholm, aged 65 or older, who did not have a history of dementia; individuals younger than 65 were excluded because 96 percent of dementia diagnoses occur in the 65-and-over age group.
After a follow-up period of approximately four years, 7 percent of the study participants developed some form of dementia.
Even after accounting for kidney function and other factors, researchers found that albuminuria was associated with a higher risk of developing dementia.
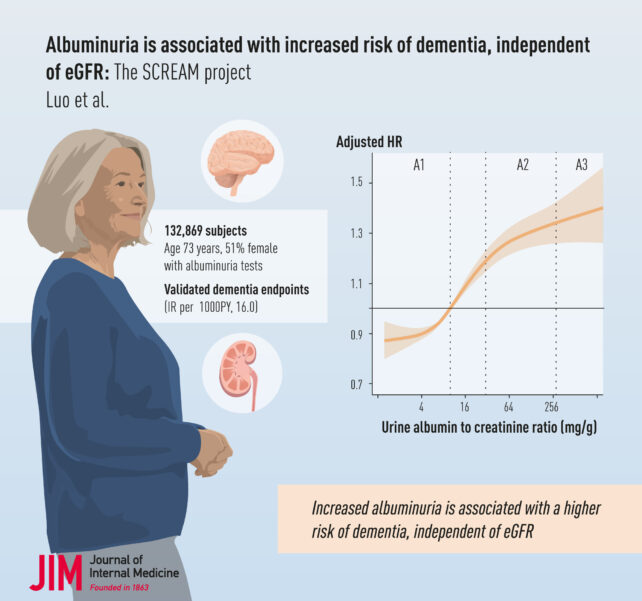
Compared to people with normal levels (<30 mg/g) of albumin in their urine, those with moderate levels (30–299 mg/g) displayed a 25 percent higher chance of developing dementia, while individuals with high levels (≥300 mg/g) had a 37 percent greater risk.
What's the potential connection? To alter an old saying, as below, so above – just as albuminuria is a marker of kidney damage, it can signal the same type of blood-vessel-related damage in the brain.
"The kidneys and the brain may seem like very different organs, but they share an important characteristic: both depend on a delicate network of small blood vessels," explains Hong Xu, nephrologist at the Karolinska Institutet in Sweden, and the study's corresponding author.
"When the blood vessels in the kidneys are damaged, the same process often occurs in the brain."
Accordingly, albuminuria was most strongly associated with vascular dementia, which is linked to vascular causes like hypertension, diabetes, or stroke. Vascular dementia is the second-most common form of dementia, behind Alzheimer's disease, which comprises 60-80 percent of all cases.
So, what seem like dissimilar processes may mirror each other in mechanism. As kidney damage allows protein to leak into urine, damage in the brain allows toxic, inflammatory molecules to leak into brain tissues.
Normally, this is prevented by the blood-brain barrier, which acts like a bouncer at a nightclub, keeping out biological riff-raff and preventing toxins from infiltrating the brain.
But defects or damage in the blood-brain barrier lead to neurological issues like inflammation, vascular damage, and a build-up of abnormal proteins that are linked with the progression of dementia.
This apparent association also corroborates past evidence. A Norwegian cohort and a population-based US study previously noted that individuals with increased albumin in their urine showed a significantly higher risk of developing dementia.
Going forward, albuminuria screening can provide an invaluable tool for assessing early dementia risk, especially for patients with comorbidities like diabetes, hypertension, cardiovascular disease, or kidney disease.
The benefits of more precise screening strategies may be profound: "Early detection of albuminuria could potentially delay or prevent the onset of dementia," explains Xu.
Future study could focus on the associations between albuminuria and specific dementia subtypes, as each subtype differs in risk factors, progression, and treatments.
Additionally, this study highlights that participants' cultural origins may be relevant during screening. Earlier studies have suggested that individuals from 'Eastern' and 'Western' cultures display different cognitive processes and may therefore perform differently on cognitive tests used to gauge dementia.
Since dementia cannot (yet) be cured, the onus is now on increasing preventive measures by identifying salient risk factors.
Crucially, this study can help introduce a more modern, synergistic way of exploring the causes of neurodegenerative diseases by assessing the links between organ dysfunction, brain chemistry, and neurological well-being.
This research is published in the Journal of Internal Medicine.
