New research shows that people who take certain psychiatric medications may be more likely to develop amyotrophic lateral sclerosis (ALS), which is the most common form of motor neurone disease (MND).
This study, which was led by a team from the Karolinska Institute in Sweden, raises some important questions about the connections between psychiatric symptoms, ALS, and MND, and how they might be targeted for treatment.
Anxiolytics, hypnotics and sedatives, and antidepressants are the most commonly prescribed drugs for psychiatric disorders such as anxiety, depression, and sleep problems. In terms of increased ALS risk, it worked out as 34 percent, 21 percent, and 26 percent respectively for the three drug types.
The increased risk is extremely small when taken in context with the low prevalence of ALS itself. Yet understanding these links could help improve our understanding of motor neurone disease and provide insights for specialists prescribing ways to treat common psychiatric disorders.
"In this case-control study, prescribed use of anxiolytics, hypnotics and sedatives, or antidepressants was associated with a higher subsequent risk of ALS," write the researchers in their published paper.
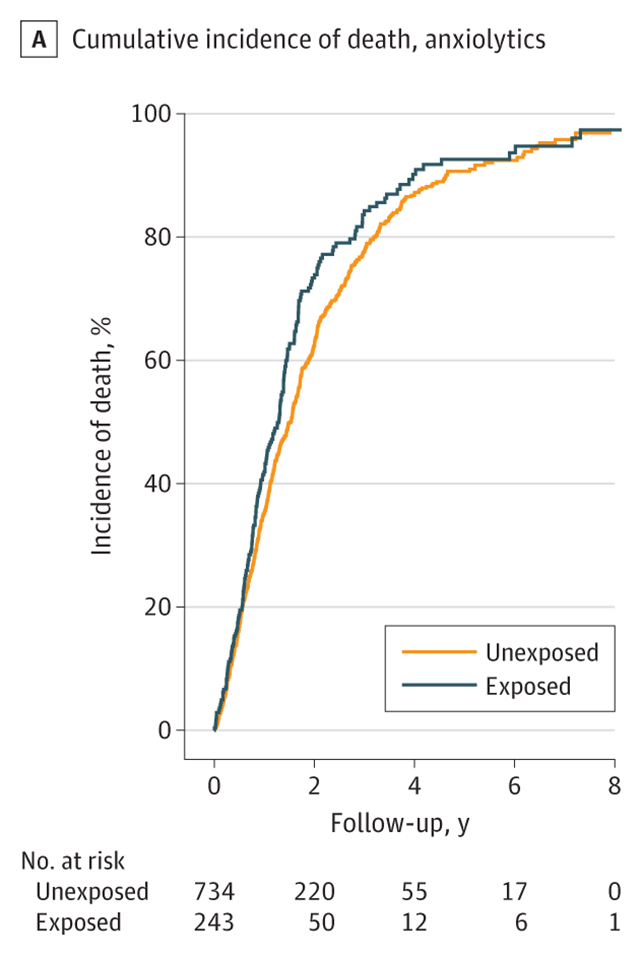
"Prediagnostic use of such medications was also associated with a poor prognosis after ALS diagnosis."
At the moment, there's no cure for the progressive debilitation that ALS causes, as parts of the nervous system break down – leading to paralysis and, eventually, respiratory failure.
The team also identified a slight increase in rate of decline and risk of an earlier death among those diagnosed with ALS who had been exposed to one of a number of psychiatric medications.
The researchers used national health data in Sweden to compare 1,057 people with ALS who had been diagnosed between 2015 and 2023 with more than 5,000 controls matched for age and sex who had no MND diagnosis.
The researchers also accounted for genetic and environmental factors in their analysis, further backing up the idea that the increased risk of ALS was connected to the medication – or the reasons the medications were prescribed.
The data isn't enough to show the drugs are directly causing the increase in ALS risk. It's also possible that other health-related factors are causing both the prescription of psychiatric medications, and the higher likelihood of an ALS diagnosis.
"This study adds to growing evidence that individuals with psychiatric conditions may face an elevated risk of neurodegenerative diseases such as ALS," says neuroscientist Susannah Tye, from the University of Queensland in Australia, who was not involved in the study.
"However, the implication that psychiatric medications themselves contribute to this risk should be interpreted with caution."
Given that previous research has found people with psychiatric disorders are also more at risk of developing ALS, these results may provide some much needed detail to the overall picture of how these different conditions, and their causes and treatments, fit together.
It's worth noting that ALS remains a rare condition, affecting around 9 in 100,000 people in the US. Depression and anxiety are much more common, which means millions of people take these medications to treat their mental health without ever developing ALS.
Over time though, scientists are gradually understanding the different factors that affect ALS risk, which should provide clues as to how it might one day be effectively treated.
The research has been published in JAMA Network Open.
