A new study suggests fat deposits in the brain may play a larger role in Alzheimer's disease than previously thought. This could open a new avenue for potential treatment.
Research has long focused on proteins found abnormally clumping in brains with neurodegeneration, but targeting these clumps has so far produced mixed results. So some researchers continue to search for missing components in our Alzheimer's disease model.
"In our view, directly targeting plaques or tangles will not solve the problem; we need to restore function of immune cells in the brain," explains Purdue University chemist Gaurav Chopra.
Related: The Cause of Alzheimer's Could Be Coming From Within Your Mouth
This is based on recent research revealing that immune cells, such as astrocytes and microglia, are being disrupted by associated fat molecules. The amyloid beta protein clumps may themselves be a symptom of the same issue, not a direct cause.
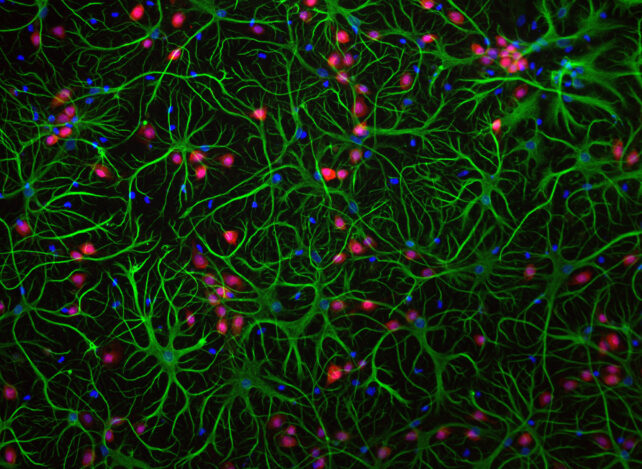
So in their new study, neuroscientist Priya Prakash and colleagues investigated what's happening with the fats in these cells using images of brain tissue from Alzheimer's patients.
They found that when these support cells are near amyloid beta plaques – within 10 micrometers – they accumulate so many lipids that their plaque-clearing rate drops by 40 percent compared to healthy microglia.
"We showed that amyloid beta is directly responsible for the fat that forms inside microglia," says Chopra. "Because of these fatty deposits, microglial cells become dysfunctional – they stop clearing amyloid beta and stop doing their job."
The researchers then identified the enzyme causing this excessive fat storage: DGAT2. And this could provide a new potential target for treatment.
"What we've seen is that when we target the fat-making enzyme and either remove or degrade it, we restore the microglia's ability to fight disease and maintain balance in the brain – which is what they're meant to do," explains Chopra.
An increasing number of people face cognitive decline, either personally or in loved ones, with almost 10 million new cases of dementia globally each year. Despite decades of research, treatment outcomes remain unclear, so exploring new tactics like this is essential to improving lives, but there's still a long way to go.
"By pinpointing this lipid burden and the DGAT2 switch that drives it, we reveal a completely new therapeutic angle," says Purdue University neuroimmunologist Palak Manchanda.
"Restore microglial metabolism and you may restore the brain's own defense against disease."
This research was published in Immunity.