A new drug has been shown to significantly reduce cancer cells in almost 80 percent of patients with an advanced form of leukaemia in a four-year clinical trial. In 20 percent of patients, it caused complete remission of the disease.
"Many patients have maintained this response more than a year after their treatment began, and some patients remain in remission more than four years on," said Andrew Roberts, one of the trial leaders working with the Royal Melbourne Hospital and the Walter and Eliza Hall Institute in Australia. "This is a very exciting result for a group of people who often had no other treatment options available."
The new drug, Venetoclax, is taken in tablet form, and was given in varying doses to 116 patients in Australia and the US over a four-year period. The patients tested had advanced cases of chronic lymphocytic leukaemia (CLL) that all other conventional treatment options had failed to improve.
Despite their bleak prognosis at the beginning of the trial, 79 percent of the patients had their cancer cells reduced by at least half. Impressively, 20 percent went into remission, and had such a profound response that the most sensitive tests couldn't detect any remaining leukaemia cells in their bodies.
To say that the trial was successful is an understatement. "These results set the foundation for building towards the dream of cure for CLL," said John Seymour, a haematologist involved in the trial at the Peter McCallum Cancer Centre in Melbourne.
Based on the results, which have been published in The New England Journal of Medicine, Venetoclax has now been given Priority Review status by the US Federal Drug Agency (FDA) for treating certain cases of CLL. That status is only given to medications that the FDA deems as having the potential to provide significant improvements in the diagnosis, treatment, or prevention of a disease.
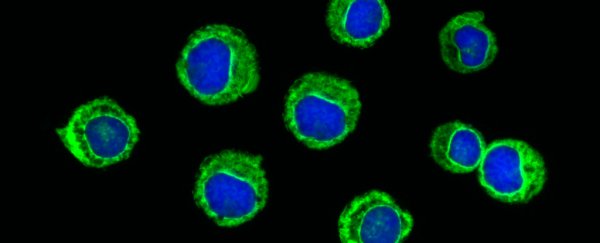
The drug achieved such impressive results by targeting a protein called BCL-2, which was shown in the 1980s to promote cancer cell survival. Venetoclax is the first class of drug that's been developed specifically to block the action of BCL-2.
"High levels of BCL-2 protect the leukaemia cells from dying, so the leukaemia can grow and become resistant to standard treatments," said Roberts. "Venetoclax selectively targets the interaction responsible for keeping the leukaemia cells alive and, in many cases, we've seen the cancerous cells simply melt away."
In a field where many of the most promising treatments in the lab often end up failing in clinical trials, it's an incredibly exciting result. But the drug isn't perfect, which is why it's only being ear-marked for patients who have run out of other options.
Side effects experienced by some patients during the trials included nausea, pneumonia, diarrhoea, respiratory tract infections, anaemia, and prostate cancer. Some patients reported no side effects at all.
That doesn't sound great, but when all other treatments have failed, it's something patients might be willing to risk in order to greatly reduce their leukaemia cells.
CLL is one of the most common forms of leukaemia, with more than 14,000 people being diagnosed with the disease in the US in 2015, and more than 4,000 being killed by it.
"The fact that a targeted drug, given on its own, can produce such a profound reduction in the leukaemia burden in the patent, to the point we cannot find the leukaemia even with our best tests, underscores what a powerful strategy targeting the BCL-2 gene is," said Seymour.
"That potential for broader application and the fact that this is a completely new class of drugs takes this beyond simply being a very good outcome for patients," he told The Sydney Morning Herald.
Phase 2 and 3 trials are now underway to test the drug against a range of blood cancers globally.