By harnessing light, my colleagues and I designed a wireless, ultrathin pacemaker that operates like a solar panel. This design not only eliminates the need for batteries but also minimizes disruptions to the heart's natural function by molding to its contours.
Our research, recently published in the journal Nature, offers a new approach to treatments that require electrical stimulation, such as heart pacing.
Pacemakers are medical devices implanted in the body to regulate heart rhythms. They're composed of electronic circuits with batteries and leads anchored to the heart muscle to stimulate it.
However, leads can fail and damage tissue. The location of the leads can't be changed once they're implanted, limiting access to different heart regions. Because pacemakers use rigid, metallic electrodes, they may also damage tissue when restarting the heart after surgery or regulating arrhythmia.
Our team envisioned a leadless and more flexible pacemaker that could precisely stimulate multiple areas of the heart. So we designed a device that transforms light into bioelectricity, or heart cell-generated electrical signals.
Thinner than a human hair, our pacemaker is made of an optic fiber and silicon membrane that the Tian lab and colleagues at the University of Chicago Pritzker School of Molecular Engineering have spent years developing.

Unlike conventional solar cells that are usually designed to collect as much energy as possible, we tweaked our device to generate electricity only at points where light strikes so it can precisely regulate heartbeats. We did this by using a layer of very small pores that can trap light and electrical current. Only cardiac muscles exposed to light-activated pores are stimulated.
Because our device is so small and light, it can be implanted without opening the chest.
We were able to successfully implant it in the hearts of rodents and an adult pig, pacing the beats of different heart muscles. Because pig hearts are anatomically similar to human hearts, this accomplishment shows our device's potential to translate to people.
Why it matters
Heart disease is the leading cause of death around the world. Annually, over 2 million people undergo open-heart surgery to treat heart problems, including to implant devices that regulate heart rhythms and prevent heart attacks.
Our ultralight device gently conforms to the surface of the heart, enabling less invasive stimulation and improved pacing and synchronized contraction. To reduce postoperative trauma and recovery time, our device can be implanted with a minimally invasive technique.
What still isn't known
Currently, our technology is best first used for urgent heart conditions, including restarting the heart after surgery, heart attack and ventricular defibrillation. We continue to explore its long-term effects and durability in the human body.
The body's internal environment is rich in fluids that are disturbed by the heart's constant mechanical motion. This could potentially compromise the device's functionality over time.
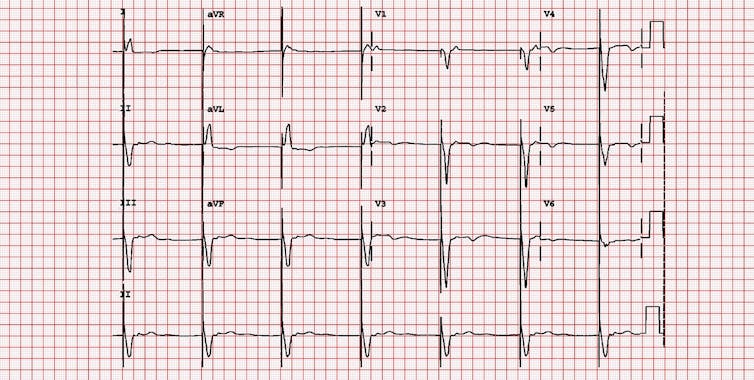
Michael Rosengarten BEng, MD.McGill/EKG World Encyclopedia via Wikimedia Commons, CC BY-SA
Moreover, researchers don't fully understand how the body reacts to prolonged exposure to medical devices. The formation of scar tissue around the device after implantation can diminish its sensitivity. We are developing special surface treatments and biomaterial coatings to decrease the likelihood of rejection.
Although the breakdown of our device results in a nontoxic substance the body can safely absorb called silicic acid, evaluating how the body responds to extended implantation is essential to ensure safety and effectiveness.
What's next
To achieve long-term implantation and tailor the device to each patient, we are refining the rate at which it dissolves naturally in the body. We are exploring enhancements to make the device compatible as a wearable pacemaker. This involves integrating a wireless light-emitting diode, or LED, beneath the skin that is connected to the device via an optical fiber.
Our ultimate goal is to broaden the scope of what we call photoelectroceuticals beyond cardiac care. This includes neurostimulation, neuroprostheses and pain management to treat neurodegenerative conditions such as Parkinson's disease.
The Research Brief is a short take on interesting academic work.![]()
Pengju Li, Ph.D. Candidate in Molecular Engineering, University of Chicago Pritzker School of Molecular Engineering
This article is republished from The Conversation under a Creative Commons license. Read the original article.
