Every three seconds, someone in the world develops dementia. Alzheimer's disease is the most common form of dementia, accounting for between 60% and 70% of all cases.
Although scientists have made significant progress in understanding the disease, there's still no cure. That's partly because Alzheimer's disease has multiple causes – many of which are still not fully understood.
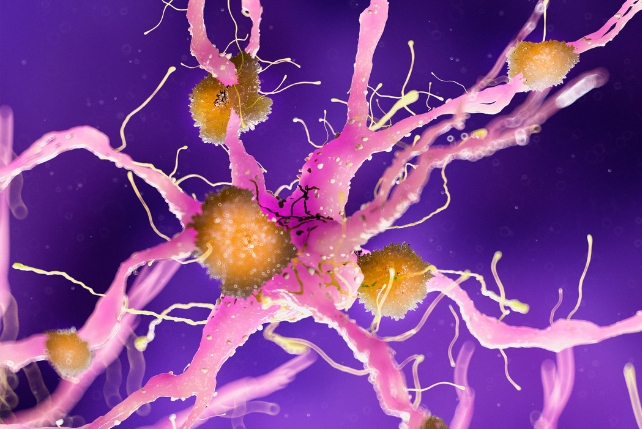
Two proteins which are widely believed to play central roles in Alzheimer's disease are amyloid-beta and tau. Amyloid-beta forms sticky plaques on the outside of brain cells. This disrupts communication between neurons.
Tau accumulate inside brain cells, where it twists into tangles. This ultimately leads to cell death. These plaques and tangles are the hallmark features of Alzheimer's disease.
This understanding, known as the amyloid hypothesis, has shaped research for decades and led to treatments that aim to clear amyloid from the brain. Monoclonal antibody drugs have been approved in recent years for this purpose.
But they only work in the early stages of the disease. They do not reverse existing damage and may cause serious side-effects such as brain swelling and bleeding. Most importantly, they only target amyloid-beta, leaving tau untreated.
But in a surprise twist, recent research published by my colleagues and me has found that a protein from Helicobacter pylori – a bacteria best known for causing stomach ulcers – can block the toxic buildup of both amyloid-beta and tau.
This unexpected finding may point to a new strategy for the fight against Alzheimer's disease.
Our discovery began with a very different question. We were initially studying how H pylori interacts with other microbes. Some bacteria form protective communities called biofilms, which rely on amyloid assemblies (similar in structure to the plaques which form in the brain) as a structural scaffold.
This led us to wonder: could H pylori influence bacterial biofilms by also interfering with amyloid assemblies in humans?
We turned our attention to a well-known H pylori protein called CagA. While half of the protein is known to trigger harmful effects in human cells (referred to as the C-terminal region), the other half (the protein's N-terminal region) may have protective properties.
To our surprise, this N-terminal fragment, called CagAN, dramatically reduced the formation of both bacterial amyloids and biofilms in the bacterial species Escherichia coli and Pseudomonas.
Encouraged by these results, we tested whether the same protein fragment could block the buildup of human amyloid-beta proteins.
To do this, we incubated amyloid-beta molecules in the lab: some were treated with CagAN, while others were left as normal. We then tracked amyloid formation using a fluorescence reader and an electron microscope.
We found that treated samples had far less amyloid clump formation during the testing period. Even at very low concentrations, CagAN almost completely stopped amyloid-beta from forming amyloid aggregates.
To understand how CagAN worked, we used nuclear magnetic resonance (which allows us to look at how molecules interact with each other) to examine how the protein interacts with amyloid-beta.
We also used computer modelling to investigate possible mechanisms. Remarkably, CagAN also blocked tau aggregation – suggesting it acts on multiple toxic proteins involved in Alzheimer's disease.
Blocking the disease
Our study has shown us that a fragment from the Helicobacter pylori protein can effectively block the buildup of the two proteins that are implicated in Alzheimer's disease. This suggests that bacterial proteins – or drugs modelled after them – could someday block the earliest signs of Alzheimer's.
What's more, the benefits may extend beyond Alzheimer's disease.
In additional experiments, the same bacterial fragment blocked the aggregation of IAPP (a protein involved in type 2 diabetes) and alpha-synuclein (linked to Parkinson's disease). All of these conditions are driven by the accumulation of toxic amyloid aggregates.
That a single bacterial fragment could interfere with so many proteins suggests exciting therapeutic potential. Though these conditions affect different parts of the body, they may be linked through cross-talk between amyloid proteins – a shared mechanism that CagAN could help disrupt.
Of course, it's important to be clear: this research is still at an early stage. All of our experiments were conducted in lab settings, not yet in animals or humans. Still, the findings open a new path.
Our study also uncovered the underlying mechanisms for how CagAN blocked the amyloid-beta and tau from forming amyloid aggregates.
One of the ways in which CagAN did this was by preventing the proteins from coming together to form clumps. They also prevented small, premature amyloid aggregates from forming as well. In the future, we will continue the detailed mechanism study and evaluate the effects in animal models.
These results also prompt a question: could H pylori, long seen only as harmful, also have a protective side? Some studies have hinted at a connection between H pylori infection and Alzheimer's disease, though the relationship remains unclear.
Our discovery adds a new layer to this discussion, suggesting that part of H pylori may actually interfere with the molecular events that lead to Alzheimer's disease.
That means in the future, we may need to take a more precise and personalised approach. Instead of aiming to eliminate H pylori completely with antibiotics, it might be more important to understand, in different biological contexts, which parts of the bacterium are harmful, and which might actually be beneficial.
As medicine continues to move toward greater precision, the goal may no longer be to wipe out every microbe, but to understand how some of them might work with us rather than against us.![]()
Gefei Chen, Associate professor, Karolinska Institutet
This article is republished from The Conversation under a Creative Commons license. Read the original article.
