The looming threat of antibiotic resistance means we desperately need new remedies to counter deadly superbugs, and researchers could have just found one in the most natural food source of all: breast milk.
Scientists have long known that, in addition to general sustenance, breast milk offers babies vital nutrients to build up their immune systems. Now, researchers have discovered a new mechanism behind this antibacterial boost – in breast milk sugars.
Contrary to the understanding that antibacterial defences are passed from mothers to their babies solely through proteins in breast milk, a team from Vanderbilt University says sugars – or carbohydrates – also demonstrate properties that can protect against bacterial infections.
"This is the first example of generalised, antimicrobial activity on the part of the carbohydrates in human milk," says chemist Steven Townsend.
"One of the remarkable properties of these compounds is that they are clearly non-toxic, unlike most antibiotics."

The most prominent infection that affects newborns is called Group B Streptococcus (GBS), which can lead to babies developing sepsis or pneumonia before their immune systems are strong enough to fight off the bug.
Luckily, while GBS can be deadly for babies, most newborns don't get infected by it, and the team wanted to investigate whether those infants might be getting protection courtesy of their mothers' milk.
"We wondered whether [GBS's] common host, pregnant women, produces compounds that can either weaken or kill strep, which is a leading cause of infections in newborns worldwide," Townsend explains.
To find out, the researchers took human breast milk carbohydrates from five human donors and isolated complex sugars from them (called oligosaccharides), before introducing the oligosaccharides to strep cultures in the lab.
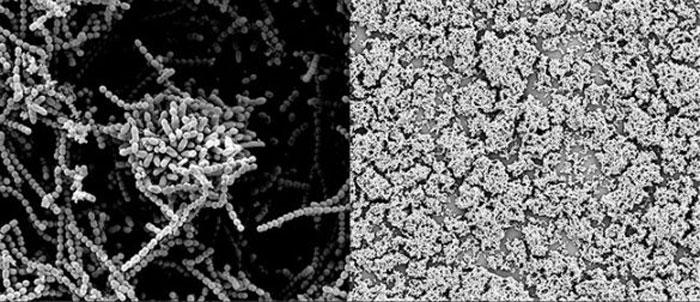
Analysing the interaction under microscope, the team found the carbohydrate could both kill the bacteria as well as weaken its natural defences – by preventing it from forming a protective biofilm to fend off threats.
 Steven Townsend/Vanderbilt
Steven Townsend/Vanderbilt
In the image above, that biofilm can be seen on the left – but it's prevented from forming in the presence of the carbohydrates (on the right).
"When bacteria want to harm us, they produce this gooey protective substance," Townsend explains, "which allows them to thwart our defence mechanisms."
In one sample, the sugars killed the strep entirely. In another, they were moderately effective at killing the strep, while in the remaining three samples the carbohydrates weren't very effective.
To help explain what's going on here, the team is currently conducting another set of tests.
In new research not yet published but presented this week at a meeting of the American Chemical Society in Washington, DC, Townsend's group again found a mix of results.
These included two cases where breast milk sugars broke down the biofilm and killed the bacteria; four where the biofilm was broken but the bacteria survived; and two where the bacteria died, but the biofilm persisted.
It's early days, and it's clear that more research will be needed to figure out the spectrum of these outcomes.
But if the team can solve the puzzle, it could lead to the beginnings of a new class of antibiotics, now that we know how these carbohydrates function in the presence of bacteria.
"[T]hese sugars have a one-two punch," says Townsend.
"First, they sensitise the target bacteria and then they kill them. Biologists sometimes call this 'synthetic lethality' and there is a major push to develop new antimicrobial drugs with this capability."
In addition, the team says its preliminary, still-in-progress data indicates that milk sugars can make bacteria more susceptible to common antibiotics – such as penicillin and erythromycin.
We shouldn't get too carried away until the team has more to show, but if those results pan out, it's possible that the carbohydrates might be able to one day lessen our reliance on these kinds of common antibiotics, and in doing so help to unravel a big part of the resistance problem.
We won't know more until the latest research is complete, but it's a hugely promising direction to investigate further – and one that, one day, could reap benefits for everybody.
"If you can figure out how the sugars are acting, then you can justify attempting to make large-scale amounts of them," Townsend says, "and then putting them in humans."
The findings are reported in Infectious Diseases.
