There's new hope for improved brain cancer treatments after scientists noticed unexpectedly positive effects coming from an unlikely source – a drug normally used to treat malaria.
The anti- malaria drug chloroquine has now been used as a last resort on three brain cancer patients, and in each case, it seems to have overcome the cancer's resistance to traditional treatments.
Chloroquine appears to break down the defences that tumours develop in response to cancer-fighting drugs by effectively 'resetting' their vulnerability to treatment.
"We have treated three patients with the combination, and all three have had a clinical benefit," says paediatric oncologist Jean Mulcahy-Levy from the University of Colorado.
"It's really exciting - sometimes you don't see that kind of response with an experimental treatment."
One of the patients is 26-year-old Lisa Rosendahl, who was previously given just a few months to live. The aggressive glioblastoma in her brain had become resistant to chemotherapy and other targeted treatments.
Rosendahl was eventually put on a cancer inhibitor called vemurafenib, but as often happens with that particular drug, the tumour in her brain soon adapted to become resistant to it, too.
That led the staff working on Rosendahl's case to try a different approach - targeting a separate cellular process called autophagy.
Autophagy is a normal process inside the body whereby dead or damaged cells are removed and recycled to make way for fresh ones. Taken from Greek, the term literally means "to eat oneself", and it's an important way of detoxifying and repairing the body.
The trouble is, tumours sometimes use autophagy to stay healthy, leveraging cellular recycling to withstand the stress that drugs put them under. Rosendahl had a type of cancer that was especially dependent on the process, due in part to a genetic mutation called BRAFV600E.
Fortunately, chloroquine is known to inhibit autophagy, so with that in mind, Mulcahy-Levy and her team decided to give the drug a try as a last-ditch effort to combat the tumours - by combining it with vemurafenib.
"Miraculously, [Rosendahl] had a response to this combination," says Mulcahy-Levy. "Four weeks later, she could stand and had improved use of her arms, legs, and hands."
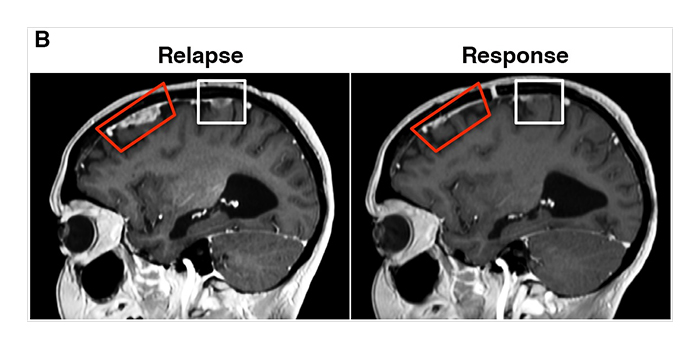 One of the scans showing the tumour (highlighted) shrinking after treatment. Credit: University of Colorado
One of the scans showing the tumour (highlighted) shrinking after treatment. Credit: University of Colorado
The chloroquine didn't remove the tumour, but it did weaken the cancer's defences enough to get the vemurafenib drug working again to do that on its own, and now Rosendahl's quality of life is improving.
Only three patients have been given the treatment so far, and not every type of cancer relies so much on autophagy, so until it's been tested on a much larger and diverse sample, it's too soon to tell if it will have similar effects on other patients.
But the team says a wider clinical test could be rolled out quickly, because chloroquine is already approved as a safe anti-malaria drug by the US FDA (Food and Drug Administration).
The researchers hope that future studies will reveal other cancers where this treatment could be effective.
"It makes me feel really lucky to be a pioneer in this treatment," says Rosendahl. "I hope it helps and I hope it helps people down the road. I want it to help."
The latest findings have been published in eLife.
