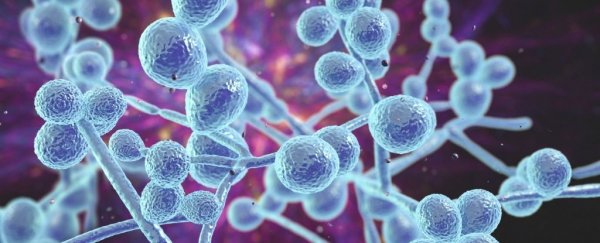
Some strains of yeast in the human gut can produce toxins that could contribute to irritable bowel disease (IBD), according to new research.
These "high-damaging" Candida albicans yeast strains aren't usually a problem when they are kept in balance, but in the guts of those with IBD, the fungi appear to proliferate, triggering inflammation.
The research was focused on a form of IBD known as ulcerative colitis (UC), which is marked by inflammation and frequent ulceration of the lining in the large intestine. In this part of the gut, fungi are also highly abundant and rich in diversity.
When scientists compared the colons of 40 UC patients against 38 controls who didn't have IBD, they found C. albicans strains were over-represented in the guts of those with UC.
The more severe the case, the more likely the patient was to show a higher abundance of Candida in their colon.
To test how these strains impact inflammation, researchers turned to mouse models. In mice without colon inflammation, the yeast strains identified in humans did not proliferate. But in mice with colon inflammation, mimicking UC, the yeast did.
Looking closer, researchers realized some yeast strains were producing a potent toxin called candidalysin, which can damage immune cells, triggering further inflammation.
Even when the sickest mice were given steroids, a common prescription for UC, the "high-damaging" strains of gut fungi continued secreting toxins, which could explain why current IBD treatments often fail to resolve symptoms.
"Our findings suggest that C. albicans strains do not cause spontaneous intestinal inflammation in a host with intact immunity," says Iliyan Iliev from Weill Cornell Medicine at Cornell University in the US.
"But they do expand in the intestines when inflammation is present and can be a factor that influences response to therapy in our models and perhaps in patients."
In other words, for most people, C. albicans strains are not a problem. Even the ones that produce cell-damaging toxins can also help the immune system. In the gut of someone with UC, however, where inflammation is widespread, some of these yeast strains seem to take off, causing more harm than good.
However, it's still up for debate which comes first, the toxins or the inflammation.
"We do not know whether specific strains are acquired by specific patients during the course of disease or whether they have been always there and become a problem during episodes of active disease," says Iliev.
"Nevertheless, our findings highlight a mechanism by which commensal [that is, internal cohabitants] fungal strains can turn against their host and overdrive inflammation."
In the lab, scientists found the candidalysin toxin produced via yeast can damage specific immune cells, known as macrophages. In turn, this can trigger a storm of cytokines, which are proteins that promote inflammation via the immune system.
In mice, toxin-producing yeast induced an expansion of T-cells and white blood cells called neutrophils, which can both drive inflammation and lead to tissue damage.
Neutrophils are often more abundant in those with active IBD, and the new results suggest their presence could be tied to a rise in fungal toxins. When researchers blocked the cytokine signaling pathway that kicks neutrophils into action in mouse models, it reduced overall colon inflammation.
This signaling pathway could thus provide drug makers a target for future IBD treatments. Direct antifungal therapies could also prove useful.
Compared to the microbiota, which is the gut's community of microbes, there is very little research out there on the fungi in our intestines, known as the mycobiota.
In fact, between 2008 and 2018, there were almost a hundred times more peer-reviewed publications on the microbiota than the mycobiota.
Recent research suggests that is an oversight. Bacteria and fungi in the gut have similar effects on the immune system, as well as nutrition; they can interact, too. Some forms of bacteria, for instance, appear to keep C. albicans in check.
While past studies have drawn a connection between the mycobiota and IBD, this is one of the first studies to dig into the mechanism behind this relationship.
The authors are now working on several follow-up studies to see how toxin-producing yeast inflames the colon and to figure out which patients will respond best to antifungal treatments.
The study was published in Nature.