Infection with a common parasite can seriously disrupt the brain function of intermediate hosts – potentially including humans – new research has found.
Even when the number of neurons affected is relatively small, toxoplasmosis – infection with the parasite Toxoplasma gondii – strongly interferes with neuronal communication. That's revealed by a study involving mouse brain cells, some grown in a dish and some collected from living animals.
Neurons infected with the parasite release fewer extracellular vesicles (EVs), tiny lipid-bound packets of proteins, nucleic acids, and metabolites that are used as a means of intercellular communication. It's a finding that carries a lot of weight in the debate on the behavioral impact of toxoplasmosis.
Related: Parasites May Be Hijacking Evolution on Planet Earth
"We found this disruption in EV signaling can interfere with how neurons and glial cells, especially astrocytes, maintain a healthy brain environment," says parasite immunologist Emma Wilson of the University of California Riverside School of Medicine.
"Even a handful of infected neurons can shift the brain's neurochemical balance. This suggests that communication between neurons and supporting glial cells is not only critical, but also vulnerable to hijacking by parasites."
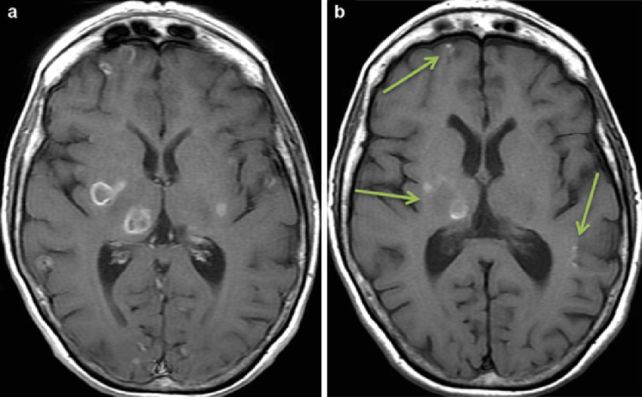
T. gondii is a parasite known for wreaking behavioral changes – for better or worse – in its hosts. It likes to find a cell and nestle inside, and the types of cells it likes most are neurons, crossing the blood-brain barrier to get there. Once inside, the protozoan can hunker down for decades, just hanging out.
It's one of the most successful parasites on the planet, and there are few warm-blooded species it can't invade. However, it can only reproduce in cats; research suggests that some of the behavioral changes exhibited by infected organisms are to force them into an increased likelihood of encountering cats, such as rodents suddenly wanting to seek out the smell of cat pee instead of avoiding it.
Some studies have found that the evidence for such behavioral manipulation is circumstantial, and that we can't conclusively link these changes to the parasite. It's especially complicated for humans; behavior is complex, and it's difficult to attribute changes to any one cause.
The new study isn't behavioral, but entirely based on physical evidence. The researchers infected mouse neurons with T. gondii, and carefully analyzed the production and content of EVs, comparing it against EV production in healthy, uninfected neurons.
They found that not only was EV production reduced, the content of the packets was altered compared to those produced by healthy neurons. Since the role of EVs is to relay information between neurons and astrocytes, this had a knock-on effect: the astrocyte gene expression was also altered, resulting in increased production of specific immune signatures, and a decrease in a transporter that helps remove excess glutamate from the brain.
Excess glutamate is linked to problems such as seizures and neural damage, complications that are known to arise from severe cases of toxoplasmosis. This suggests that we might be underestimating the impact of T. gondii.
"The parasite may play a larger role in neurological and behavioral conditions than we previously thought," Wilson says.
A shockingly large number of humans harbor T. gondii. It's mostly contracted from ingesting poorly prepared food, such as undercooked meat, or from interacting with cat feces. Prevalence rates reach as high as 80 percent in some parts of the world; in the US, an estimated 10 to 30 percent of the population is infected.

Most people will never know about their little neural hitchhikers and will sail through life unaffected, but for some people – particularly infant, elderly, immunocompromised, and pregnant people – infection can become dangerous.
The most effective prevention tools are to cook your meat thoroughly, wash your vegetables, and wash your hands carefully after handling kitty litter. Meanwhile, research such as Wilson's may help us better understand the parasites, and work on ways of protecting ourselves.
"Our brains have built-in defenses that may recognize and respond to neurons infected by T. gondii," she says. "If we can learn how to support or enhance that process, we may be able to better protect people, especially the most vulnerable."
The research has been published in PLOS Pathogens.
