The surgical removal of the uterus and both ovaries may come at a serious and overlooked cost to individual health, new research suggests.
A meta-analysis of data from research on over 2 million people has found that having a hysterectomy to remove the uterus and cervix is linked to a 5 percent higher risk of stroke than not having the surgery.
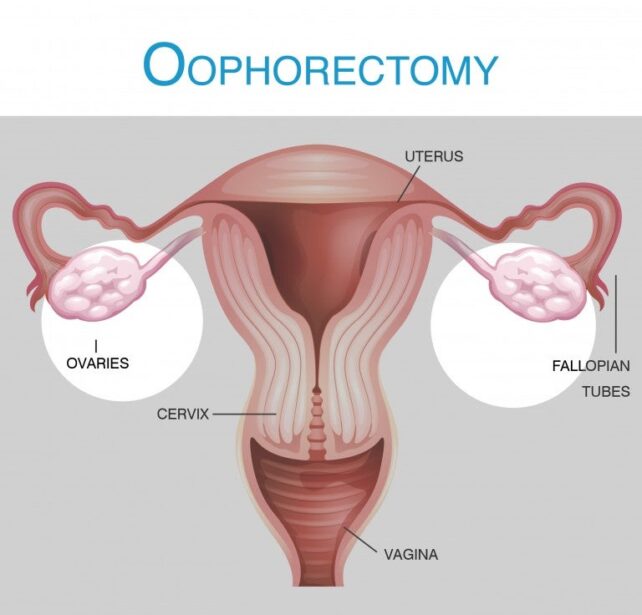
What's more, having a hysterectomy along with the removal of both ovaries is linked to an 18 percent higher risk of stroke. The removal of both ovaries is called a bilateral oophorectomy.
Related: Having Both Ovaries Removed Could Come at a Serious Cost to The Brain
"The results… [highlight] that these common procedures carry longer-term risks," says Stephanie Faubion, medical director for The Menopause Society, a nonprofit organization that seeks to improve women's health.
"They also call attention to an opportunity for more careful assessment of cardiovascular risk and implementation of risk reduction strategies in women who undergo these surgeries."
Today, hysterectomies and oophorectomies (removal of one or both ovaries) are some of the most common surgical procedures that women receive in the US, and yet we still know very little about the long-term health effects.
While many of these surgeries are conducted for non-terminal conditions, recent evidence suggests that they could come at a life-threatening cost to the body and brain.
Recommendations differ, but typically, hysterectomies are reserved as a last resort for serious gynecological conditions, like cancer, prolapse, endometriosis, postpartum hemorrhage, or uterine fibroids.
Before the turn of the century, however, it was relatively common practice in the US to remove both ovaries during a hysterectomy. Only in recent decades has evidence suggested that this approach comes with potential dangers.
A large-scale study from 2009 found that women who had both their ovaries removed as part of a hysterectomy for benign disease faced a significantly increased risk of dying from any cause, including coronary heart disease and lung cancer.
Compared to those who retained their ovaries, those who had them removed faced a 14 percent higher risk of stroke.
The reason behind the association is unclear, but some scientists suspect that because the ovaries release hormones, these outcomes are linked to premature menopause.
Today, the removal of both ovaries is generally not recommended in pre-menopausal patients unless they face serious risks, like cancer.
But the link between oophorectomies and stroke is complex, and it could be influenced by factors like age at the time of surgery, the use of hormone replacement therapy, and various definitions of stroke.
In 2018, for instance, some researchers found that young women who have an oophorectomy and use estrogen replacements are not necessarily at an increased risk of stroke.
In 2024, however, a meta-analysis revealed the opposite, finding hysterectomy was associated with stroke risk, especially when both ovaries were removed.
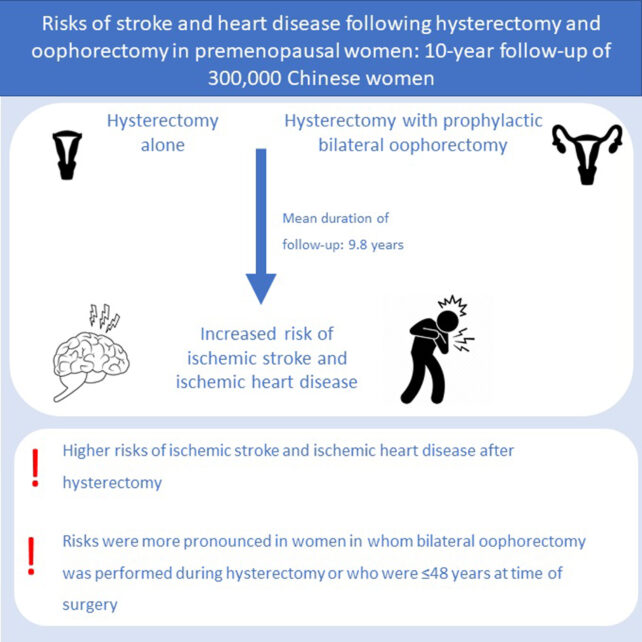
To clear up confusion, researchers in China analyzed long-term national health data from the US, collected from more than 21,000 women between 1999 and 2018. They then combined this research with 15 other studies for statistical comparison.
Analyzing the national data from 1999 to 2018, it seemed that hysterectomy was not significantly associated with stroke risk. It was only associated with an elevated risk if both ovaries were removed as well.
However, in the larger meta-analysis the data did demonstrate an increased risk for both groups. This suggests that some previous studies may be underpowered to reliably detect a significant association, requiring larger sample sizes.
"The current study indicates that hysterectomy and/or bilateral oophorectomy are associated with an increased risk of stroke, underscoring that women who have had these surgeries should be closely monitored and require proactive preventive health measures for early signs of stroke," the authors of the recent meta-analysis conclude.
"Moreover, our findings encourage clinical researchers to explore new safer surgical techniques or alternative treatments for diseases related to hysterectomy/bilateral oophorectomy."
The study was published in Menopause.