Ten years ago, an unnamed American woman was diagnosed with HIV. Like the tens of thousands of people who test positive in the US each year, she faced a lifetime of anti-retroviral therapies to keep the virus from obliterating her immune system.
Today, that's no longer the case.
The patient is part of an extremely exclusive club of individuals who appear to have purged the virus entirely from their bodies. What's more, the means to her cure gives hope to dozens of patients like her each year.
A team of researchers in the US working as part of the International Maternal Pediatric Adolescent AIDS Clinical Trials Network (IMPAACT) recently reported the middle-aged patient to be virus-free more than four years after a revolutionary treatment for blood cancer.
Just two other cases of total HIV remission have ever been satisfactorily confirmed, both following transplants of bone marrow from donors with HIV-blocking mutations in treatment of leukemia.
One, a Caucasian male known as the "Berlin patient", was in remission for more than a decade before passing away in 2020 from his cancer. The other, a Latino male dubbed the "London patient", has been virus-free now for more than two years.
Just like these two renowned patients, the woman at the center of this latest case was also diagnosed with a blood cancer. In 2017, tests confirmed she had acute myelogenous leukemia (AML), a life-threatening condition affecting bone marrow.
Had the woman been White, she would have had a higher chance of finding a tissue match within the Caucasian-dominated library of willing donors.
Instead, given her mixed-race heritage, specialists turned to another source of stem cells that could potentially provide the seeds for new, healthy bone marrow – umbilical cord blood.
Unlike most tissue transplants, blood from a newborn's umbilicus doesn't require a perfect immunological match between the host and donor. Since the 1990s, more than 35,000 leukemia patients around the world have received a cord blood donation.
While it's a prime choice of treatment for AML, cord blood takes weeks to settle in and generate sufficient white cells to keep infections at bay. This makes it a rather poor option for anybody dealing with a persistent deadly infection.
To circumvent this problem, the patient's medical team devised a two-pronged strategy – receive infusions of blood from a compatible relative to provide her with a temporary defense, and cord stem cells that can slowly generate white cells.
As an added fortune, the cord cells the patient received came with a bonus talent. Their DNA carried two copies of the CCR5 delta-32 mutation.
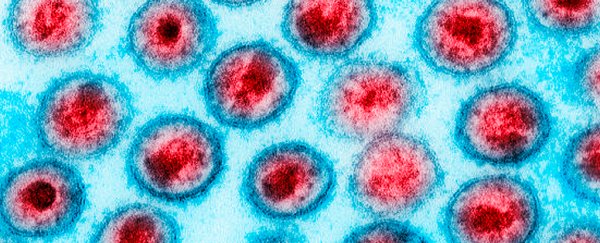
This small genetic difference alters the expression of the CCR5 co-receptor, the doorway most strains of HIV use to gain entry into the body's cells. Without easy access into white blood cells, the virus can't slide inside and destroy them.
Around three months after her transplant, all of the patient's T white blood cells and myeloid cells (white cells that gobble up invaders) were derived not from her old marrow, or her relative's blood, but from the stem cells in the cord blood.
That means they all featured the protective version of the CCR5 co-receptor, locking out her HIV for good.
Since then the patient has stopped all anti-retroviral medication, showing no signs of active HIV particles.
Cord blood stem cells have a lot going for them as a form of leukemia therapy, compared with more traditional forms of blood stem cells from a donor. For one thing, there appears to be a reduced risk of relapse.
What's more, side-effects that are common among marrow transplants, such as graft versus host disease, are less likely. In fact, the patient in this case left hospital just 17 days after her treatment.
Most excitingly, the fact that umbilical cord blood is more forgiving in terms of compatibility between donors and hosts means people from diverse ethnic and racial backgrounds could at last be eligible.
The researchers presented their preliminary findings at the 2022 Conference on Retroviruses and Opportunistic Infections, though are yet to publish or make their research publicly available.
For now, the study poses an exciting possibility for curing a fraction of the people with HIV – an ongoing pandemic that currently affects almost 40 million people around the globe.
This isn't to say this new therapy would be available to all people living with HIV, at least not any time soon. The risks involved still mean it's an option only available for treating life-threatening blood cancers, with the chance of curing HIV a prospective bonus.
But for those handfuls of eligible patients hit with both a cancer and HIV diagnosis, it's a thin silver lining that gives hope for a slightly brighter future.