Scientists have developed a vaccine against a notorious drug-resistant superbug, targeting molecules on its surface that are also found on other bacteria and fungi.
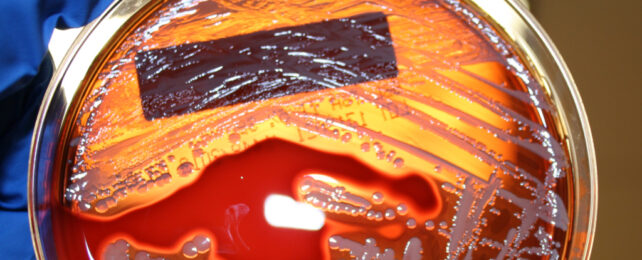
Although only tested in mice, the vaccine offers high levels of protection against Staphylococcus aureus, a species of bacteria found in people's noses but also causing skin and blood infections, and its relative, methicillin-resistant Staphylococcus aureus (MRSA).
Bacterial vaccines aren't easy to develop. As of December 2022, 94 bacterial vaccine candidates were in animal trials, and another 61 were in clinical development. But at the time of that review, a vaccine against S. aureus was considered unlikely and unfeasible.
That's not for lack of trying. S. aureus is one of the World Health Organization's priority pathogens due to its presence in hospitals, and a bunch of S. aureus vaccines have been tested without much success.
Part of the challenge is that S. aureus is particularly well-endowed with cell surface decorations and has many ways of evading the immune system. As a result, an effective vaccine would probably have to target multiple parts of the bacterium at once, so it can't escape.
Vaccines against bacterial infections have also been largely overlooked in favor of more immediate or probable solutions to antibiotic resistance, such as prescribing antibiotics more wisely, developing new classes of antibiotics that target pathogens in different ways, and reducing their use in livestock.
But despite those efforts and some successful bacterial vaccines, antibiotic resistance remains a growing threat and urgent problem. In 2019, bacterial antimicrobial resistance ranked as the third leading cause of death worldwide.
MRSA is of particular concern, causing infections in hospitals, prisons, and nursing homes, but also in the general community.
"There are worries that at the rate things are going, in perhaps 20 or 30 years, few of our drugs will be effective at all," says Michigan State University chemist Xuefei Huang, who led the research group behind this latest study. "This would bring us back to the pre-antibiotic age."
Vaccines, however, could help us get ahead of the problem, stopping infections and thereby reducing the need for antibiotics to treat them. "This reduces the chance for bacteria to develop resistance, breaking the cycle," Huang explains.
For their vaccine, Huang's team focused on a molecule called Poly-β-(1–6)-N-acetylglucosamine (PNAG), a carbohydrate found on the cell wall of Staphylococcus known to aid immune evasion.
Bacteria are typically covered in carbohydrates, chemical compounds composed of sugars, and while each could represent a new target for vaccines, they also complicate the picture.
Also found on many other bacteria and even fungi (which are rising up as another massive threat to global health), a critical section of the PNAG structure is highly variable among different pathogens, making it hard to target.
Huang's team created a library of 32 different PNAG structures, which had different molecular groups adorning their common sugary backbone. The effect of these side groups on S. aureus' interactions with the immune system is not well understood.
"We wanted to know: Was there a best combination to improve Staph aureus vaccine efficiency, and does the arrangement matter?" Huang explains.
Two combinations looked particularly promising and could be easily synthesized. But PNAG and other carbohydrates don't typically provoke strong immune responses in humans. So the team modified a bacteriophage, a virus that only infects specific bacteria, so it could carry hundreds of PNAG structures and boost immune responses to the vaccine.
Testing the PNAG-loaded bacteriophage in mice, the researchers found the vaccine provided animals with "near complete protection" against S. aureus infections, including MRSA.
The new vaccine construct also outperformed another PNAG-vaccine delivery system that is currently in human trials, producing higher levels of protective antibodies in mice. Antibody levels remained high one year after immunization, and could be boosted back to peak levels after nearly two years, suggesting the vaccine could provide lasting protection.
Of course, much more research is needed to test whether this new vaccine candidate works in larger animals and possibly humans, is safe, and at what doses. There's a long way to go yet.
The research has been published in Nature Communications.