A deadly superbug that sometimes claims the lives of more than a million people globally a year may have a nemesis that lives right under your nose.
Quite literally. It dominates your skin microbiome, where it seems to keep staph infections at bay.
The overlooked agent is a species of natural yeast, called Malassezia sympodialis – one of the most prevalent microorganisms on healthy human skin. New research suggests that as it cleans oil and fat from your body's exterior, the fungi can produce a fatty acid that stops the development and growth of a staph infection.
According to lab experiments, led by scientists at the University of Oregon (UO), M. sympodialis can antagonize Staphylococcus aureus bacteria through its acidic byproducts.
Because the yeast-produced acid is often present in healthy skin, researchers think it stops S. aureus from over-colonizing the microbiome. S. aureus is a normal component of the skin microbiome, but if it takes over, or if it penetrates the tissue or bloodstream, it can seed dangerous infections.
Skin and soft tissue infections involving S.aureus result in approximately 500,000 hospitalizations annually in the United States, and the bacterium is capable of becoming resistant to every class of antibiotics we currently have in our arsenal.
This means new drug therapies must be continuously put forward to stay ahead of its deadly toll. The fact that our skin microbiome has natural defenses against staph infections is worth exploring further.
"There are lots of studies that identify new antibiotic structures," says lead author and evolutionary biologist Caitlin Kowalski from UO, "but what was fun and interesting about ours is that we identified (a compound) that is well-known and that people have studied before."
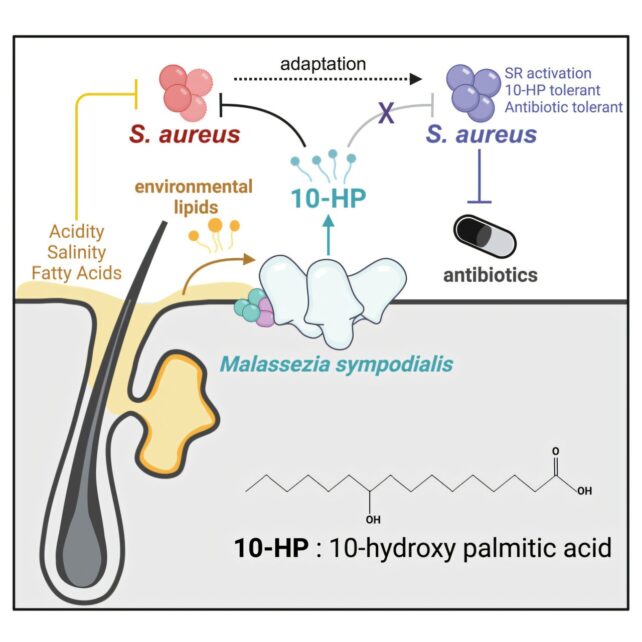
The compound in question is called 10-hydroxy palmitic acid (10-HP), and in the past, scientists probably overlooked its antimicrobial powers because it only unleashes its toxic effects in a low pH environment, like the skin, and not under normal lab conditions.
Using human skin biopsies from healthy donors, Kowalski and colleagues found the acid was produced by resident Malassezia yeast.
"It was like finding a needle in a haystack but with molecules you can't see," says Kowalski's adviser, biologist Matthew Barber.
In the lab, Barber, Kowalski, and their colleagues tested how M. sympodialis yeast impacts various strains of S. aureus. After two hours of the yeast treatment, most S. aureus strains showed greater than a 100-fold reduction in viability.
Over time, S. aureus strains developed some resistance to M. sympodialis' 10-HP, and the dangerous bacteria did so in a similar way to how they develop tolerance to clinical antibiotics.
Interestingly, researchers found that other species of Staphylococcus bacteria, which do not pose the same threat as S. aureus, had already figured out similar ways to coexist with the M. sympodialis yeast.
"Given the prevalence of Malassezia within the mammalian skin microbiota, we are likely just scratching the surface of its roles in shaping microbial interactions and colonization resistance in this niche," write the authors.
Kowalski is now planning to do a deep dive into the genetic mechanisms of antibiotic-resistant staph infections to better understand how the bacteria rapidly mutates to avoid a whole range of antimicrobial agents.
"We still have a lot of work to do in understanding the microorganisms, and also finding new ways that we can possibly treat or prevent those infections," says Barber.
The study was published in Current Biology.
