Antibiotic resistance is causing us all sorts of havoc. It's turning once manageable pathogens into superbugs, hitting our most vulnerable people the hardest.
Superbugs were involved with nearly 5 million deaths globally in 2019, so antibiotic resistance is generally not something we at all want to promote in the slightest.
But while it's boosting our bacterial nemeses, resistance factors mean our good bacteria are becoming more resistant to antibiotics as well.
A new study has found antibiotic resistance genes is also giving our gut bacteria an advantage, allowing them stay on top in their never ending battle against microbes that cause us harm.
"Antimicrobial resistance mutations in commensals can have paradoxically beneficial effects by promoting microbiome resilience to antimicrobials," University of Massachusetts bioinformatician Shakti Bhattarai and colleagues write in their paper.
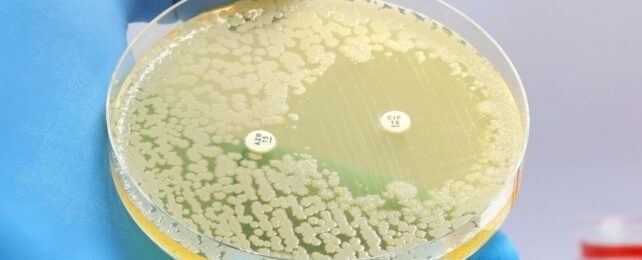
The researchers investigated the war between good and bad gut bacteria within 24 patients who have multidrug-resistant tuberculosis (Mycobacterium tuberculosis), detailing the battle in a blow-by-blow account. The patients had received numerous types of antibiotics to keep their illness at bay, a regime they were required to maintain for 20 months.
Treatment initially devastated their gut microbiomes, causing disruptions in the metabolism, composition, and diversity of bacterial species.
Unpleasant side effects included diarrhea and gut inflammation, which isn't surprising given antibiotic use has also been linked to increased cases of irritable bowel syndrome.
Yet over time, something rather surprising was observed among the patients.
"Our findings document an unexpected resilience of the microbiome to disruption by long-term antibiotics," write the researchers, explaining how the microbiomes in the patients spontaneously reestablished the dominance of friendly bacteria in the wake of initial imbalance.
What's more, they found the state of the patient's gut microbiome as well as the clearance of the tuberculosis bacteria itself are linked to recovery from tuberculosis-driven inflammation. Blooms of bacteria from the Enterobacteriaceae family post-treatment led to more widespread inflammation, whereas microbiomes with more Clostridia and fewer Enterobacteriaceae were associated with a faster drop in the inflammation that drives tuberculosis symptoms.
Further tests in mice involving fecal transplants from the patients revealed their microbiomes had acquired a resistance to subsequent antibiotic disruption. These resistance genes were still seen in some of the friendly bacterial species a year after antibiotic treatments had ceased in the mice.
"These mutations may have a fitness benefit in the microbiome ecosystem established by long-term antibiotics," the team explains, suggesting we may be able to use this in some way to counter the antibiotic resistant pathogens.
While this may of course risk more antibiotic resistance, and requires a heck of a lot more research before being seriously considered, it may be a risk worth taking if it allows our friendly bacteria to outcompete them, Bhattarai and colleagues conclude.
This research was published in Science Translational Medicine.