The role of the gut microbiome in causing Alzheimer's disease has finally been confirmed.
Using gut microbiota transplants, an international team of researchers has shown memory impairments in humans with Alzheimer's can be passed on to young, healthy rats.
The study also revealed specific bacteria in the gut are directly linked to cognitive decline in Alzheimer's patients.
This highlights the gut microbiome as a key area of research for Alzheimer's and other forms of dementia, and that could lead to new ways to treat the disease.
"People with Alzheimer's are typically diagnosed at or after the onset of cognitive symptoms, which may be too late, at least for current therapeutic approaches," says neuroscientist Yvonne Nolan from University College Cork (UCC) in Ireland.
"Understanding the role of gut microbes during prodromal – or early stage- dementia – before the potential onset of symptoms may open avenues for new therapy development, or even individualized intervention."
Evidence has recently pointed to changes in the gut microbiota as a potential risk factor for the development of Alzheimer's, though whether they were merely associated in some way wasn't clear. Now we have confirmation that gut microbiota actually play a causal role in the development of symptoms of the devastating disease.
"Alzheimer's is an insidious condition that there is yet no effective treatment for," says Sandrine Thuret, a neuroscientist at King's College London (KCL). "This study represents an important step forward in our understanding of the disease."
Nolan, Thuret, and colleagues from UCC, KCL, and IRCCS Saint John of God Clinical Research Centre of Bresci in Italy set out to understand how the gut microbiota in Alzheimer's patients affects brain health and behavior.
Human participants, including 69 with Alzheimer's disease and 64 healthy controls, donated blood for research, with some from each group also providing gut microbiota via stool samples.
Gut microbiota from Alzheimer's patients was transplanted into 16 young adult rats whose microbiomes had been depleted by antibiotics for a week. A matching group of 16 rats received gut microbiota from humans in the healthy control group.
At least 10 days after the transplants, the rats were subjected to behavioral tests designed to evaluate memory performance as well as other traits associated with Alzheimer's disease.
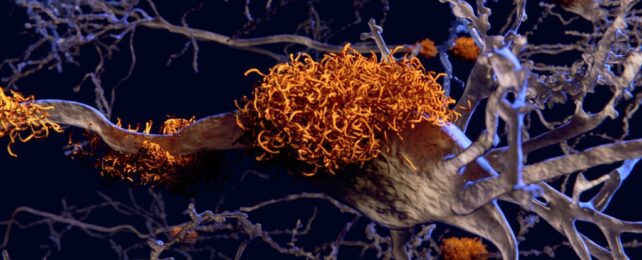
Rats that had microbiome transplants from Alzheimer's patients showed impaired memory behaviors, particularly those that rely on a process called adult hippocampal neurogenesis.
Hippocampal neurogenesis creates new neurons in the hippocampus, a region of our brains that's important for memory and mood, and one of the first areas impacted by Alzheimer's.
"The memory tests we investigated rely on the growth of new nerve cells in the hippocampus region of the brain," explains Nolan. "Animals with gut bacteria from people with Alzheimer's produced fewer new nerve cells and had impaired memory."
Rats with Alzheimer's patients' gut microbiota exhibited more severe impairments in hippocampal neurogenesis when the donors themselves had lower cognitive test scores.
The researchers also saw clear modifications in the rats' hippocampal metabolome – the collection of metabolites such as amino acids and enzymes that are involved in the maintenance, growth, and normal function of cells. These changes might contribute to the decreased growth of new neurons in the hippocampus.
Hippocampal neurogenesis can't be measured so easily in living humans, but blood from Alzheimer's patients decreased neurogenesis in human neural stem cells in the laboratory.
Levels of gene expression in stem cells exposed to blood of Alzheimer's patients were also linked to how well the patients performed on cognitive tests, and the types of bacteria in their guts.
"Impaired neurogenesis may be the converging link between the observed altered gut microbiota composition and cognitive impairment in Alzheimer's disease," the team writes.
Bacteria from the genus Coprococcus, which are associated with healthy aging, were significantly reduced in Alzheimer's patients. They also had significantly more bacteria from the Desulfovibrio genus than cognitively healthy controls, similar to past research in animal models of Alzheimer's, and Parkinson's disease.
Future studies should thoroughly assess other aspects that affect gut microbiota, like health status, lifestyle factors, and medication history, according to the team.
"This collaborative research has laid the groundwork for future research into this area," Thuret says, "and my hope is that it will lead to potential advances in therapeutic interventions."
The study has been published in the journal Brain.