Identifying early signs of Alzheimer's gives the best chance of slowing its progression, with researchers previously finding clues of the disease in a person's speech and breathing, and in gut bacteria.
Now a new study says a dwindling sense of smell may be one of the earliest indicators of the condition, arriving even before cognitive impairments.
Related: 5 Early, Speech-Related Signs You're at Risk of Alzheimer's Disease
While previous research has identified olfactory deficits as a possible early warning of Alzheimer's, the mechanisms have remained unclear.
In the new research, scientists sought to uncover the neural underpinnings of the disease, analyzing positron emission tomography (PET) scans and brain tissue samples from mice as well as humans.
Their findings suggest the brain's immune response plays a key role in the loss of smell linked to Alzheimer's, seemingly killing off neuronal fibers the brain needs for odor perception.
Specialized immune cells in the brain known as microglia sever connections between the olfactory bulb and the locus coeruleus, the study found.
The olfactory bulb is a forebrain structure that receives and analyzes signals from scent receptors in the nose, then sends the information to other parts of the brain for processing.
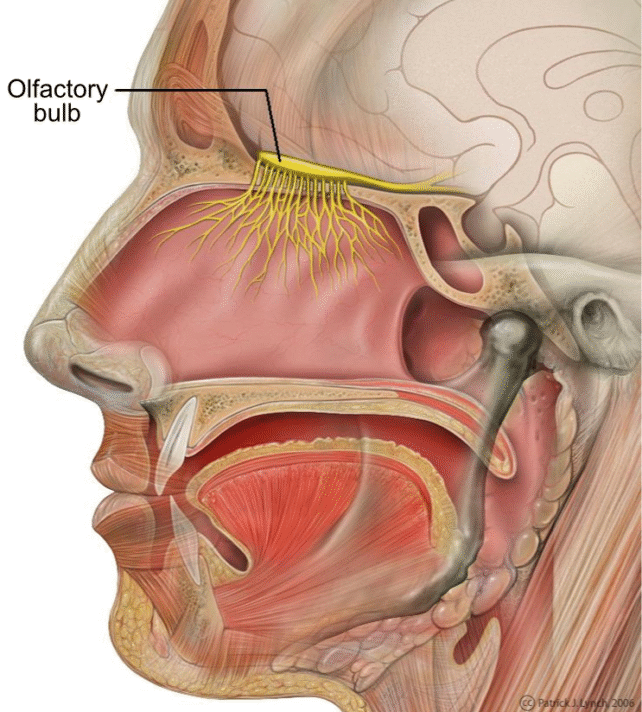
The locus coeruleus is in the brainstem, but it influences the olfactory bulb and other brain areas via long nerve fibers, explains neurobiologist Lars Paeger from the German Center for Neurodegenerative Diseases (DZNE) and Ludwig Maximilian University of Munich (LMU).
"The locus coeruleus regulates a variety of physiological mechanisms. These include, for example, cerebral blood flow, sleep-wake cycles, and sensory processing," he says. "The latter applies, in particular, also to the sense of smell."
In early stages of Alzheimer's disease, pivotal changes occur along those nerve fibers linking the locus coeruleus to the olfactory bulb, the new study suggests.
"These alterations signal to the microglia that affected fibers are defective or superfluous," Paeger says. "Consequently, the microglia break them down."
The changes occur in the membranes of neurons, where a fatty acid known as phosphatidylserine – typically located inside the membrane – has moved to the exterior. That's likely what drew attacks by microglia.
"Presence of phosphatidylserine at the outer site of the cell membrane is known to be an 'eat-me' signal for microglia," Paeger says. "In the olfactory bulb, this is usually associated with a process called synaptic pruning, which serves to remove unnecessary or dysfunctional neuronal connections."
This fatty acid's relocation may occur because Alzheimer's disease is already causing the nerve cells to behave differently.
"In our situation, we assume the shift in membrane composition is triggered by hyperactivity of the affected neurons due to Alzheimer's disease," Paeger says. "That is, these neurons exhibit abnormal firing."
The study took a multipronged approach, studying live and dead mice with features of Alzheimer's, post-mortem brain tissue from human Alzheimer's patients, and PET brain scans of people with Alzheimer's or mild cognitive impairment.
"Smell issues in Alzheimer's disease and damage to the associated nerves have been discussed for some time. However, the causes were unclear," says neuroscientist Joachim Herms from DZNE and LMU.
"Now, our findings point to an immunological mechanism as cause for such dysfunctions – and, in particular, that such events already arise in the early stages of Alzheimer's disease."
Since those initial stages are so important for Alzheimer's treatment, shedding light on the loss of smell may yield valuable information to help more people catch the disease in the early going.
"Our findings could pave the way for the early identification of patients at risk of developing Alzheimer's, enabling them to undergo comprehensive testing to confirm the diagnosis before cognitive problems arise," Herms says.
"This would allow earlier intervention with amyloid-beta antibodies, increasing the probability of a positive response."
The study was published in Nature Communications.
