A daily cup of coffee could be blunting the effects of certain antibiotic treatments, according to a new study analyzing the reaction of Escherichia coli bacteria to caffeine.
The international team of researchers behind the study looked at 94 different chemical substances and how they changed E. coli: specifically, how they altered the systems that control what gets into and out of the bacterial cells.
Around a third of the substances tested were shown to interfere with gene activity related to managing traffic in and out of the cell. But caffeine was the one that stood out. It led to the E. coli absorbing a lower level of some antibiotics, including ciprofloxacin.
"Our data show that several substances can subtly but systematically influence gene regulation in bacteria," says microbiologist Christoph Binsfeld, from the University of Würzburg in Germany.
Related: Coffee Can Mess With Your Medication. A Pharmacist Explains Why.
This is part of ongoing research into what's known as low-level antibiotic resistance. Not the fully fledged kind, where bacteria adapt to resist targeted treatments directly, but subtler effects that are triggered by changes in how genes operate and the way that these bugs respond to their environment.
We already know that bacteria such as E. coli use these adaptive responses to maximize their chances of survival in whatever environment they find themselves in. What's not known are the precise biological mechanisms being used, which can tell scientists more about how bacteria pathogens stay alive and how we might beat them.
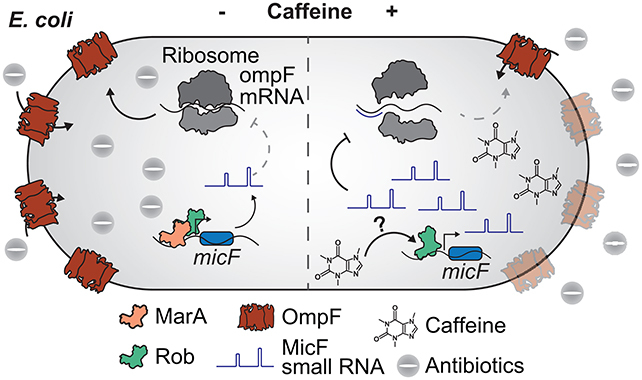
The analysis showed that a particular protein called Rob played a bigger role than previously thought in controlling what gets in and out of the bacteria cells. It was involved in about a third of all the changes spotted by the researchers, including those triggered by the introduction of caffeine.
"Caffeine triggers a cascade of events starting with the gene regulator Rob and culminating in the change of several transport proteins in E. coli – which in turn leads to a reduced uptake of antibiotics such as ciprofloxacin," says biological engineer Ana Rita Brochado, from the University of Tübingen in Germany.
It's important to note that this research is based on tests carried out in the lab: it's not fully clear how this might work in actual human beings, or how much coffee you'd actually have to drink to make a noticeable difference to antibiotic response, but this is something future research can look into.
Another discovery by the researchers was that the antibiotic weakening effect was not seen in Salmonella enterica, another harmful bacteria closely related to E. coli. This is a response that seems to only apply to certain kinds of bacteria.
There are several ways that the research can be taken forward, to get a more precise idea of what we're dealing with here, but a better understanding of this low-level antibiotic resistance is essential to making therapeutic approaches as effective as possible.
"Based on these findings, we foresee a challenging, but unavoidable and important task in mapping key determinants of transport functions across different bacteria," write the researchers in their published paper.
The research has been published in PLOS Biology.
