Imagine being infected with a deadly virus that makes you impervious to pain. By the time you realize you are infected, it's already too late. You have spread it far and wide.
Recent findings in my lab suggest that this scenario may be one reason that people infected with SARS-CoV-2, the virus causing COVID-19, may be spreading the disease without knowing it.
Most accounts to date have focused on how the virus invades cells via the ACE2 protein on the surface of many cells.
But recent studies, which have not yet been peer-reviewed, suggest there is another route to infecting the cell that enables it to infect the nervous system.
This led my research group to uncover a link between a particular cellular protein and pain – an interaction that is disrupted by the coronavirus. Our research has now been peer-reviewed and will be published in the journal PAIN.
I am a scientist who studies how proteins on cells trigger pain signals that are transmitted through the body to the brain.
When these proteins are active, the nerve cells are talking to each other. This conversation occurs at deafening levels in chronic pain.
So by studying what causes the excitability of nerve cells to change, we can begin to unravel how chronic pain becomes established. This also allows us to design ways to mute this conversation to blunt or stop chronic pain.
My laboratory has a longstanding interest in designing nonopioid-based alternatives for pain management.
Linking SARS-CoV-2 and pain
You might be wondering how my lab began to probe the connection between SARS-CoV-2 and pain.
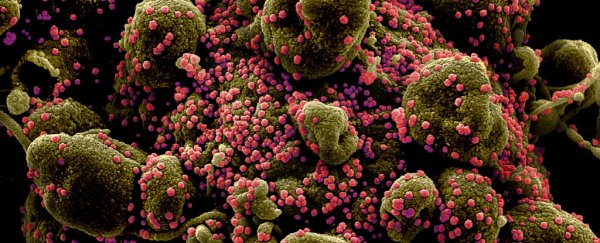
We were inspired by two preliminary reports that appeared on the preprint server BioRxiv that showed that the infamous spike proteins on the surface of the SARS-CoV-2 virus bound to a protein called neuropilin-1.
This means that the virus can also use this protein to invade nerve cells as well as through the ACE2 protein.
For the past year, some six months before the pandemic took hold, my colleagues and I had been studying the role of neuropilin-1 in the context of pain perception.
Because neuropilin-1, like the ACE2 receptor, allowed spike to enter the cells, we wondered if this alternate gateway could also be related to pain.
Under normal circumstances, the neuropilin-1 protein controls the growth of blood vessels, and as well as the growth and survival of neurons.
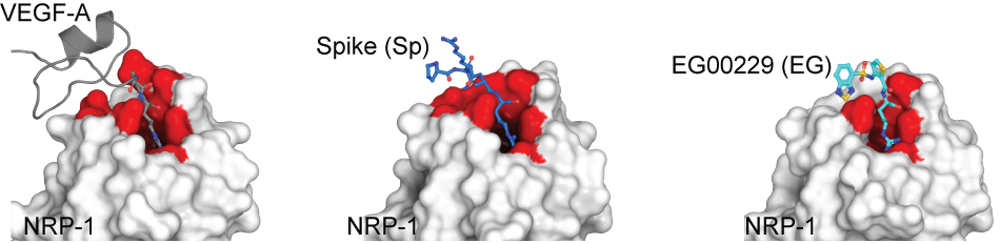
However, when neuropilin-1 binds to a naturally occurring protein called called Vascular endothelial growth factor A (VEGF-A), this triggers pain signals. This signal is transmitted via the spinal cord into higher brain centers to cause the sensation we all know as pain.
Staring at this jigsaw puzzle – neuropilin-1 and VEGF-A and neuropilin and spike – we wondered if there was a link between spike and pain.
Previous research has shown a link between VEGF-A and pain. For people with osteoarthritis, for instance, studies have shown that increased activity of the VEGF gene in fluids lubricating joints, like the knee, is associated with higher pain scores.
Although activity of the neuropilin-1 gene is higher in biological samples from COVID-19 patients compared to healthy controls and activity of the neuropilin-1 gene is increased in pain-sensing neurons in an animal model of chronic pain, the role of neuropilin-1 in pain has never been explored until now.
In in vitro studies done in my lab using nerve cells, we showed that when spike binds to neuropilin-1 it decreases pain signaling, which suggests that in a living animal it would also have a pain-dulling effect.
When the spike protein binds to the neuropilin-1 protein, it blocks the VEGF-A protein from binding and thus hijack's a cell's pain circuitry. This binding suppresses the excitability of pain neurons, leading to lower sensitivity to pain.
 (Dr Samantha Perez-Miller, CC BY-SA)
(Dr Samantha Perez-Miller, CC BY-SA)
Above: Crystal structure of neuropilin-1 b1 domain (white surface with binding site in red) showing binding of VEGF-A (left), spike protein (middle), and the neuropilin-1 inhibitor EG00229 (right).
From the COVID-19 fog a new pain target emerges
If our finding that the new coronavirus is attacking cells through a protein associated with pain and disabling the protein can be confirmed in humans, it may provide a new pathway for drug development to treat COVID-19.
A small molecule, called EG00229, targeting neuropilin-1 had been reported in a 2018 study. This molecule binds to the same region of the neuropilin-1 protein as the viral spike protein and VEGF-A.
So I and my colleagues asked if this molecule was able to block pain. It did, during pain simulations in rats. Our data reaffirmed the notion of neuropilin-1 as a new player in pain signaling.
There is precedence for targeting the neuropilin-1 protein for cancer treatment: for example, a Phase 1a clinical trial of an antibody called MNRP1685A (known under the product name Vesencumab) that recognizes and binds to neuropilin-1 and blocks VEGF-binding. This was mostly well tolerated in cancer patients, but it caused pain rather than blocking it.
Our studies identify a different approach because we targeted blocking the pain-triggering VEGF-A protein, which then resulted in pain relief.
So our preclinical work described here provides a rationale for targeting the VEGF-A/NRP-1 pro-pain signaling system in future clinical trials.
Analysis of the structure of the neuropilin-1 receptor protein may allow design of drugs targeting this critical site which also controls axon growth, cell survival – in addition to pain relief.
For instance, these neuropilin-1 receptor targeted drugs could potentially block viral infection. The testing of several candidate compounds, some of them on the FDA's generally regarded as safe list, is currently underway by my group.
Sneaky virus, fooling people into believing that they do not have COVID-19. But, ironically, it may be gifting us with the knowledge of a new protein, critical for pain.
Two roads emerge in the forest ahead: (1) block neuropilin-1 to limit SARS-CoV-2 entry, and (2) block neuropilin-1 to block pain. ![]()
Rajesh Khanna, Professor of Pharmacology, University of Arizona.
This article is republished from The Conversation under a Creative Commons license. Read the original article.