Scientists in Canada have developed a way to reprogram human blood cells into a variety of neurons, including those responsible for causing pain and numbness.
The technique will allow researchers to test new drugs for pain and other neurological conditions using millions of engineered nerve cells, which share the same genetic signature as the patient or blood donor.
"Now we can take easy-to-obtain blood samples and make the main cell types of neurological systems - the central nervous system and the peripheral nervous system - in a dish that is specialised for each patient," Mick Bhatia, director of the Stem Cell and Cancer Research Institute at McMaster University, told The Canadian Press.
"Nobody has ever done this with adult blood, ever."
When we injure ourselves, neurons in our body - comprising our peripheral nervous system - sense this pain and convey messages to the neurons in our brain. But nerve pain, not resulting from a direct injury or wound but from some kind of structural damage to the cell, is more complicated, because the messaging system isn't functioning properly.
Physicians have a limited understanding of what causes this type of pain or how to treat it, as it's difficult to runs tests on neurons. While researchers can buy certain kinds of rat neural cell lines for drug testing, these cells don't always respond to stimuli the way human neural cells do, reports the Canadian Press.
"The problem is that unlike blood, a skin sample or even a tissue biopsy, you can't take a piece of a patient's neural system. It runs like complex wiring throughout the body and portions cannot be sampled for study," Bhatia said in a press release.
This new reprogramming method provides an avenue to essentially mimic a biopsy of the brain or nervous system.
"We can actually take a patient's blood sample, as routinely performed in a doctor's office, and with it we can produce one million sensory neurons, that make up the peripheral nerves in short order with this new approach," says Bhatia. "We can also make central nervous system cells, as the blood to neural conversion technology we developed creates neural stem cells during the process of conversion."
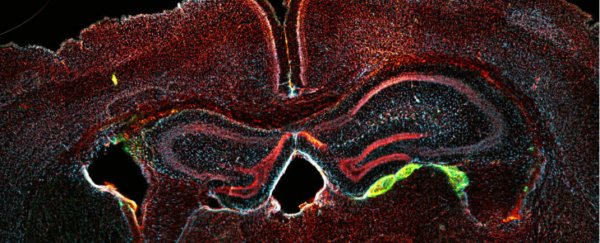
The team tested their process using fresh and frozen samples of umbilical cord and adult blood. They extracted stem cells from the blood samples, which would have evolved into either red or white blood cells. Over the course of about a month, they used a patented technique to convert them into neural progenitor cells, which can proliferate and develop into neurons found in both the brain and spinal cord, and throughout the rest of the body.
The team estimates that with just 50,000 adult blood cells, they can generate upwards of 100 million sensory neurons. They have reported their findings in the journal Cell Reports.
The researchers say the results could pave the way for the discovery of new pain drugs that don't just numb the perception of pain, but specifically target faulty neurons in the peripheral nervous system.
Bhatia says non-specific opioids used for decades, which can be addictive and have negative side effects, are still being used today.
"You don't want to feel sleepy or unaware, you just want your pain to go away," he says. "But, up until now, no one's had the ability and required technology to actually test different drugs to find something that targets the peripheral nervous system and not the central nervous system in a patient specific, or personalised manner."
In future, the team hopes to develop blood-derived neurons that might be transplanted into patients to replace degraded brain cells in people with diseases like Alzheimer's or Parkinson's.