Researchers in Germany have successfully grown the innermost layer of human fallopian tubes in the lab - the first step towards creating a functional model that will allow scientists to study how reproductive diseases such as cancer start, as well as provide important insight into the enigmatic organs.
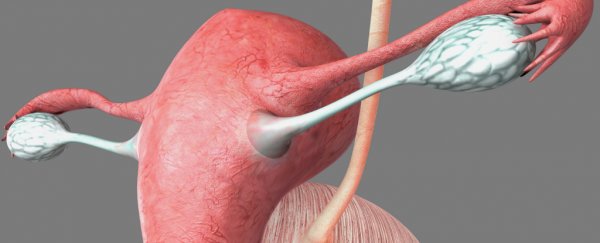
The fallopian tubes play a crucial role in the female reproductive system by connecting the ovaries to the uterus, but recent research has suggested that if fallopian tube cells become infected, they can migrate, and could be a key trigger for ovarian cancer - one of the most deadly types of female reproductive cancer.
Despite the importance of these organs, we have a lot to learn about how they function, particularly on the inside - an area that (as you can imagine) is particularly challenging for scientists to study while their patients are alive.
Which is why scientists from the Max Planck Institute for Infection Biology wanted to grow the mucous membrane epithelium that forms the inside of fallopian tubes in lab-grown replicas.
But trying to grow human organs in the lab is notoriously difficult. First of all, you need to isolate and stimulate the specific organ's adult stem cells, which are cells that are capable of differentiating into all the essential cell types needed to regenerate and maintain the organ. In this case, the researchers used fallopian epithelial cells that had stem cell-like properties taken from tissue donors.
If that doesn't sound hard enough, the researchers also had to try to replicate the environmental conditions in the human body in order to get the stem cells to grow and develop into more complex structures.
After creating special environmental conditions for their cells, the researchers noticed that some of the cells organised themselves into organoids – hollow spheres that consist of many thousands of cells and that have the characteristic structure and shape of a naturally occurring fallopian tube. Which is really, really cool.
"That happened without any additional instruction whatsoever," said one of the researchers, Mirjana Kessler. "The entire blueprint of the fallopian tube must therefore be stored in the epithelial cells."
They're a way off growing the full 10- to 15-cm organs, but testing has shown that the structure, anatomy, and biochemical processes of these organoids are very similar to those of real fallopian tubes - they even responded when the researchers added hormones to their environment.
The team has now kept the mini fallopian tubes alive in the lab for more than a year - something that could previously only be done for a few days. And they've already discovered two signalling pathways - known as Notch and Wnt - that keep the fallopian tube stem cells regenerating the organ.
On top of helping us understand how the fallopian tube grows and develops, what's more important is what this model could teach us in the future about reproductive health and cancer in women.
"With the help of our model we can now focus on determining whether cancer can be triggered by infections of the human fallopian tubes," said lead researcher Thomas F. Meyer.
While it's not the purpose of this lab group, it's also worth keeping in mind that other lab-grown organs, such as kidneys and penises, are currently being tested for human transplantation potential. Who knows, maybe one day we could see lab-grown fallopian tubes transplanted into women who are born without them, or who lose them as a result of illness or injury.
The research has been published in Nature Communications.