One in every nine people in Australia has asthma. It is a health burden for many children, and expensive for families because of medication, hospital and out-of-hospital expenses.
The pandemic has added further stress and extra testing measures to check respiratory symptoms. COVID infection can co-exist with asthma and, although research shows allergic asthma does not increase the risk of COVID infection and death, keeping asthma symptoms under control remains important.
At home, tobacco smoke, pollen, mold, dust, pet dander and harmful gases can initiate or worsen asthma symptoms. Our recent study – a review and analysis of Australian research – identifies the most significant culprits.
Passive smoking, synthetic pillows or quilts, and gas heating in your house are the most frequently identified triggers for the highest rates of asthma in the home. Preventing these common household environmental factors could better control asthma.
Nasties in the home
Prior research reports various environmental factors can trigger asthma symptoms. But the relevant factors and the size of the effect varies widely in different countries and populations. Knowing the most common environmental triggers that can initiate asthma symptoms in Australia can help us tailor prevention strategies.
We examined the evidence based on the research conducted in Australia to determine significant family environmental factors associated with asthma. We looked at 56 studies that involved 137,840 people in Australia. The combined data confirm passive smoking, synthetic bedding and gas heating in households are significant triggering factors for asthma symptoms. These household features are noted in more homes where people have asthma and need more asthma treatment.
Being around smokers, such as at home or in the workplace is the most commonly reported indoor exposure for people with asthma. Breathing in smoke disrupts normal lung and immune system development and causes airway irritation.
This can lead to asthma symptoms and other lung diseases. The main sources of secondhand smoke in Australia were identified as smoking by a parent or other family member at home and by colleagues in the workplace. Children were the main victims of secondhand smoke, exposed to their parents' smoking – especially mothers – at home.
Bedding and heating
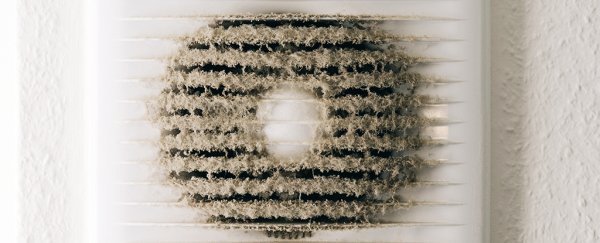
The second most commonly reported household trigger was bedding from unnatural fibers, such as microfiber, nylon or acrylic materials. Synthetic bedding items have higher house dust mite allergen levels than feather-bedding items.
They also increase exposure to volatile organic chemicals. These are gases emitted from certain solids and liquids found in many household products. These gases can accumulate in higher concentrations inside and cause health problems.
Synthetic pillows are also more likely to trap cat and dog allergens than feather pillows. The firmer weave of feather pillows makes them a more protective barrier to allergens that could otherwise lead to respiratory irritation. Households of children prone to asthma or allergies should pay extra attention to the bedding they choose.
Finally, both flued and unflued gas heaters can emit nitrogen dioxide gas that can irritate the respiratory tract and trigger asthma symptoms. It's better to get rid of gas heaters or heating systems, if possible, in households where asthma is an issue.
Asthma risks we can control
Our research shows the importance of emphasizing prevention of some common family environmental factors to prevent asthma symptoms. These factors may remain less acknowledged despite their notorious effect on asthma.
The scientific evidence that shows active tobacco smoking is detrimental for asthma control is well understood by the general public. But people may be less aware of the effect of passive smoking on asthma.
There is also scope to build awareness around gas heaters and synthetic bedding as asthma triggers. These environmental factors lurking in homes should be better communicated to families who could be affected, especially in a country where asthma is a major public health problem. Elimination of these factors may help control asthma symptoms and reduce COVID testing during the pandemic. ![]()
K M Shahunja, PhD candidate, The University of Queensland; Abdullah Mamun, Associate Professor, The University of Queensland, and Peter Sly, Director, Children's Health and Environment Program and World Health Organization Collaborating Centre for Children's Health and Environment, The University of Queensland.
This article is republished from The Conversation under a Creative Commons license. Read the original article.