When you're just a tiny parasite trying to make your way in the world, a few tricks that let you sneak into other organisms undetected are always helpful.
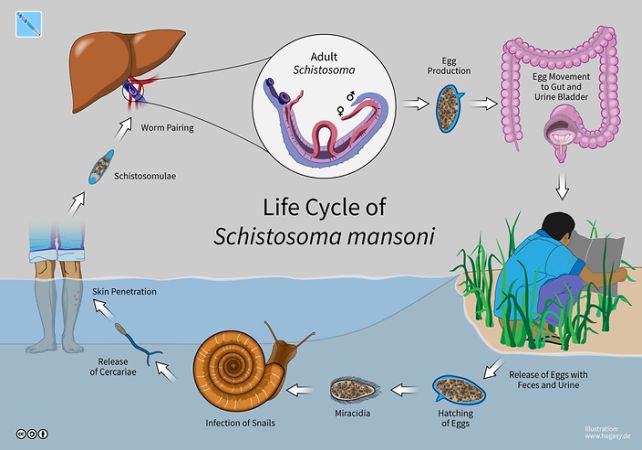
The water-borne parasitic worm (or helminth) Schistosoma mansoni has a particularly insidious lifestyle. Its larvae penetrate the skin of a host, crawling inside to the warm, moist interior of the host body, where it can grow and reproduce.
What's surprising is that this penetration causes no pain or itching, allowing it to enter undetected and cause schistosomiasis; a chronic parasitic disease that affects hundreds of millions of people around the world.
Related: Parasites May Be Hijacking Evolution on Planet Earth
Now, scientists have figured out exactly how this little worm manages to dodge the body's defenses. It produces molecules that suppress a class of neurons in the host's skin – a finding that could lead to the development of new and effective painkillers.
"If we identify and isolate the molecules used by helminths to block TRPV1+ activation, it may present a novel alternative to current opioid based treatments for reducing pain," says immunologist De'Broski Herbert of Tulane School of Medicine in the US.
"The molecules that block TRPV1+ could also be developed into therapeutics that reduce disease severity for individuals suffering from painful inflammatory conditions."
TRPV1+ neurons are a specific type of sensory neuron that sends signals such as heat, stinging, and itching as a warning signal about dangers such as noxious substances, dangerous pathogens, and allergens. The class of nerve cell also plays a role in triggering an immune response: an inflammation that would help block the S. mansoni larvae from entering the body.
The researchers hypothesized that the helminth evolved the ability to suppress the TRPV1+ neurons as a means of increasing its odds of a successful infection of its targeted host, and embarked on a study with mice to see if they were right.
They infected select groups of mice with the parasite, keeping other groups uninfected as controls. Groups were each assigned a letter, but the researchers did not know which group was infected – a study technique known as blinding that helps ensure more accurate reporting of results, compared to results that can be biased by what the scientists expect to find.
The infected and control groups were then subjected to a test to determine their pain tolerance. For each mouse, a paw was placed over a heat source – not hot enough to cause burns from a brief exposure, but hot enough to be uncomfortable. The researchers recorded how long each mouse took to withdraw its paw.
Neuron cultures were developed from the spinal fluid of both infected and uninfected mice, and capsaicin was added to study the immune response. The control group's cultures showed signs of a significantly stronger immune response than cultures from the infected group.
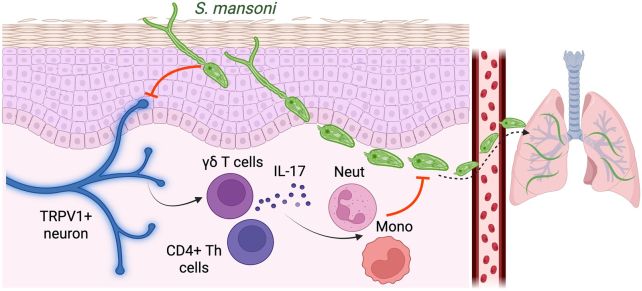
The results demonstrate that S. mansoni does indeed suppress the neurons responsible for alerting the brain to danger and eliciting an immune response that would protect against the invasion, the researchers found. While we can't be sure if it works exactly the same in humans, this opens up several possibilities for further research.
"Identifying the molecules in S. mansoni that block TRPV1+ could inform preventive treatments for schistosomiasis," Herbert says. "We envision a topical agent which activates TRPV1+ to prevent infection from contaminated water for individuals at risk of acquiring S. mansoni."
The findings could also lead to a new way to treat nerve pain, although this will require significantly more research, since immune suppression can be dangerous.
The next step in the research will to be examine in greater detail the TRPV1+-suppressing molecules secreted by S. mansoni to try to figure out exactly what they do.
The findings have been published in The Journal of Immunology.
