A hidden physical change in the body may be helping to drive the prolonged malaise some people experience after contracting COVID-19.
Analyzing blood samples from patients with long COVID, a team of medical researchers has identified unusual microscopic structures that may contribute to symptoms such as brain fog and fatigue. If this is the case, it offers a hopeful target for future treatment.
"This study shows a robust association between biomarkers indicative of thromboinflammatory activity and long COVID," the team writes in a paper led by geneticist Alain Thierry of Montpellier University in France.
"The discovery of these biomarker linkages not only presents a possible novel diagnostic methodology but also novel therapeutic targets, offering prospects for future markedly improved clinical management."
Related: We Just Got More Evidence That Long COVID Is a Brain Injury
The reason why some people experience symptoms for months to years after a SARS-CoV-2 infection is still something of a medical mystery, but multiple mechanisms may be at play.
One possibility first raised by physiologist Resia Pretorius of Stellenbosch University in South Africa in 2021 is microclots. These are tiny, abnormally persistent blood clots that are smaller than those seen in conditions such as stroke or thrombosis, yet large enough to hinder blood flow through capillaries.
Meanwhile, in 2022, Thierry and his colleagues showed that patients with long COVID have elevated levels of neutrophil extracellular traps, or NETs. These are sticky webs of DNA and enzymes released by white blood cells to capture and contain pathogens invading the body.
Normally, NETs do their job and then quickly break down, but when they are released in large numbers or persist longer than needed, they can contribute to blood flow problems such as thrombosis and atherosclerosis.
The new research – a collaboration between Pretorius and Thierry – suggests that these two separate markers, NETs and microclots, may interact in the blood of long COVID patients.
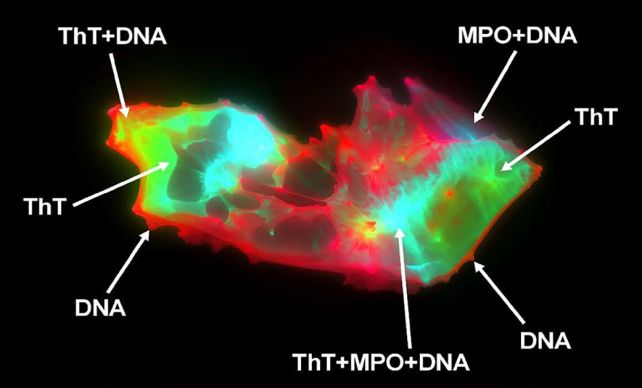
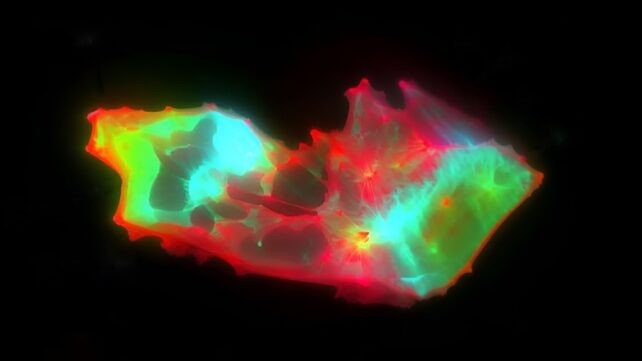
The researchers used imaging flow cytometry and fluorescence microscopy to study blood samples from 50 patients with long COVID and 38 healthy volunteers, focusing specifically on any differences in microclots and NETs. The healthy individuals had been recruited in two separate cohorts, in France and South Africa.
Patients with long COVID, the analysis revealed, had a dramatically higher number of microclots than the healthy controls – a 19.7-fold increase on the median. These clots were also larger than the microclots seen in healthy blood.
An increase in NETs also correlated with the rise in microclots in long COVID patients. But then the researchers found something new: The NETs appeared to be physically embedded within the microclots, an association that had never before been reported.
Interestingly, this association was observed in all the samples, both from the long COVID patients and control groups, which makes sense because the NETs' sticky mesh facilitates clotting.
However, the effect was much more pronounced in the long COVID group. This interaction could make the microclots more resistant to the fibrinolysis process the body uses to break up accumulations of blood material.
"This finding suggests the existence of underlying physiological interactions between microclots and NETs that, when dysregulated, may become pathogenic," Thierry explains.
So dramatic was the difference that, when the samples were anonymized, an AI agent was able to identify the long COVID patients with 91 percent accuracy. This suggests that microclots and NETs may be a biomarker that doctors could use to diagnose long COVID, a condition that has proven slippery to pin down using standard tests.
This is still early research; more work needs to be done to establish a causal relationship between microclots, NETs, and long COVID. But if researchers can figure out how these blood components affect long COVID, it may be a step towards relief for those living with the condition.
The research has been published in the Journal of Medical Virology.