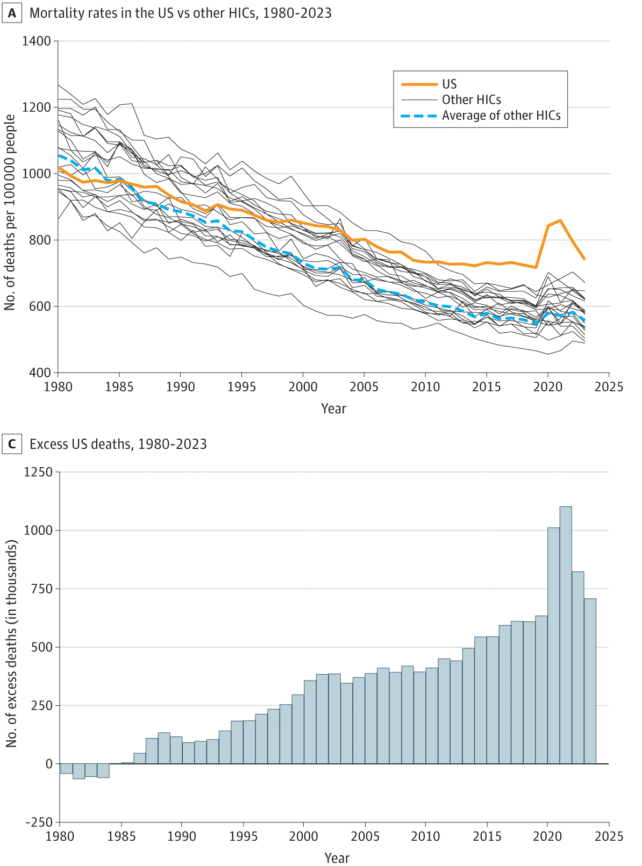
In the first years of the COVID-19 pandemic, Americans were dying at much higher rates than other wealthy nations.
A new analysis now estimates that in 2020 and 2021, more than 2 million Americans went 'missing' from the population.
These are the people who would still be alive if the US had the same death rate as other high-income nations.
To be clear, not all of these 'excess' deaths are due to COVID-19, but a significant portion are tied to the timing of the global pandemic.
"Imagine the lives saved, the grief and trauma averted, if the US simply performed at the average of our peers," says lead author and epidemiologist Jacob Bor from Boston University.
The analysis is a broad, sweeping take on a big and complicated issue, but it supports previous studies that have also found Americans suffer poor survival outcomes compared to residents in other wealthy nations.
The new study compares more than 107 million deaths of any cause in the US between 1980 and 2023 to death rates in 21 other wealthy nations. The selected countries each had a 2021 GDP exceeding US $24,000 per capita, and had data available in the Human Mortality Database spanning the study period.
Over those 43 years, the US experienced 14.7 million excess deaths relative to its peers, with a significant uptick starting in 2020.
Long before the COVID-19 pandemic began, however, data suggest health outcomes in the US were gradually slipping compared to the rest of the world.
The spread of a novel coronavirus in 2020 only widened that gap.
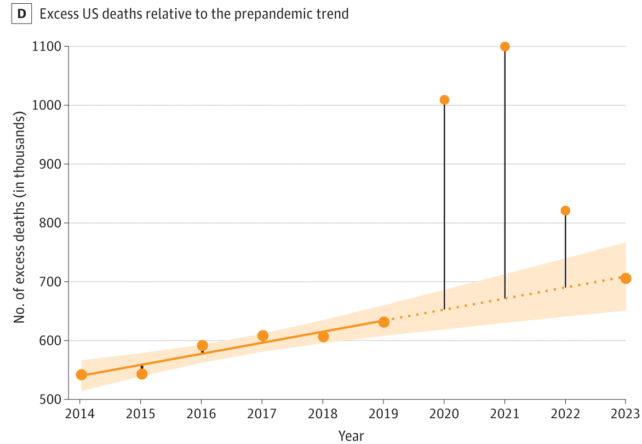
Bor and colleagues calculated that in 2019, there was a total of 631,247 missing Americans. In 2020 and 2021, that number shot up to over a million per year.
By 2022, excess deaths had slipped back to 820,396, before dropping further to 705,331 in 2023. But that is still significantly higher than in 2019.
If the US experienced the same expected death rates as other nations, the authors of the study think nearly a quarter of all deaths could have been avoided in 2023, many among younger people.
"One out of every two US deaths under 65 years is likely avoidable," says Bor.
"Our failure to address this is a national scandal."
These excess deaths are not simply due to the consequences of the coronavirus, although the pandemic certainly exacerbated the issue.
Sociologist Elizabeth Wrigley-Field from the University of Minnesota says that the increase in deaths from 2019 to 2023 is also "driven by long-running crises in drug overdose, gun violence, car collisions, and preventable cardiometabolic deaths."
In a previous study from 2023, researchers used global data to show that the US experiences excess mortality in every single age group compared to its wealthy peers.
If the US could achieve the lower mortality rates of Japan, for example, the 2023 study suggested more than 880,000 deaths could be prevented. That's comparable to eliminating all deaths from heart disease, diabetes, and unintentional injuries.
"Other countries show that investing in universal healthcare, strong safety nets, and evidence-based public health policies leads to longer, healthier lives," says senior author Andrew Stokes, demographer and sociologist at Boston University.
"These deaths reflect not individual choices, but policy neglect and deep-rooted social and health system failures. The COVID-19 pandemic exposed structural weaknesses – including gaps in healthcare access and social supports – that have continued to fuel premature deaths even after the acute phase of the pandemic ended."
The research letter was published in JAMA Health Forum.