A landmark study has identified specific patterns of connections across the brain associated with symptoms of attention deficit hyperactivity disorder ( ADHD), highlighting the importace of considering diverse neurological functions in understanding the nature of the condition.
While the study is far from unique in its attempts to identify physical characteristics of ADHD in the brain's wiring, its method does aim to improve on past efforts.
US researchers developed a new technique that provides a broad view of the brain to analyze brain scans from around 6,000 children, addressing some limitations in past research.
"Neuroimaging studies of ADHD have been hindered by small sample sizes, small effects, and differences among study methods," write bioinformatician Michael Mooney from Oregon Health & Science University and colleagues in their published paper.
Using what's known as a polyneuro risk score (PNRS) to combine small differences into brain-wide connectivity patterns, the researchers could predict ADHD symptoms in two independent cohorts. The findings could help future research into the disorder, as well as indicate a new way to study brain imaging in other neurological conditions.
ADHD is a complex neurological disorder that affects millions of children and adults. Its diagnosis is based largely on behavior, usually presenting externally as difficulties with attention, impulsivity, and sometimes hyperactivity.
Early diagnosis of ADHD can have a significant beneficial impact on the lives of patients and their families. One study found those who don't get diagnosed until adulthood are four times more likely to die early than the general population.
The disorder is often stigmatized, sometimes attributed to laziness or a lack of self-control. However, studies suggest ADHD stems from differences in how the brain functions on a structural level. The precise nature and extent of these structural differences is unclear, possibly because effects in specific parts of the brain are small, making the identification of individual neurological features a challenge.
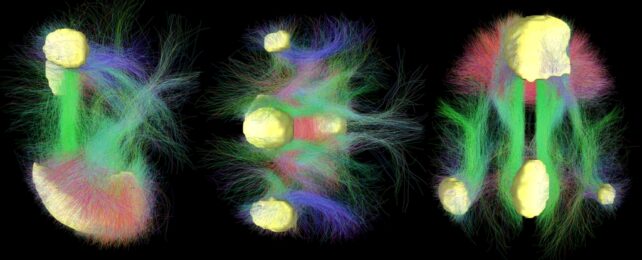
ADHD manifests differently in different people, which could be related to how different functional brain systems interact. This connectivity between functional networks can be measured via changes in blood flow in the brain while it's not focused on a task – resting-state functional connectivity MRI (rs-fcMRI).
A 2014 review of rs-fcMRI research on ADHD revealed some consistency in findings concerning the brain's default mode network. Recent meta-analysis indicated that connectivity in multiple brain networks is associated with ADHD; however most studies haven't looked at brain-wide effects.
"Given considerable evidence that ADHD is associated with alterations in widely distributed brain networks, and the small effects of individual brain features, a whole-brain perspective focusing on cumulative effects is warranted," the team writes.
The researchers constructed and validated a PNRS to represent the cumulative, total effect of brain-wide measurements of resting state functional connectivity linked to ADHD symptoms.
They used data from rs-fcMRI scans and ADHD symptom scores of 5,543 participants; children aged 9-10 years when they enrolled in the Adolescent Brain Cognitive Development Study, a long-term US study of brain development into adulthood.
The link between PNRS and ADHD symptoms was then further tested with 553 participants from the Oregon ADHD-1000 cohort, an independent dataset of people aged 7 to 11 at baseline who have annual follow up tests into adulthood.
The 'ADHD PRNS' was significantly associated with ADHD symptoms across both groups. In the Oregon group, people with an ADHD PRNS in the highest 10 percent were 3.86 times more likely to have diagnosed ADHD than those below the median.
When analysis was repeated for those with a second scan taken 1.83 years later, the strength of the link between PRNS and ADHD was almost exactly the same.
The most significant associations with ADHD were spread across multiple brain networks. The strongest effects were associated with regions that are most active when the brain is at rest, known as the default mode network; and a structure called the cingulo-opercular network, which includes areas involved in cognitive control, attention, and task monitoring.
Previous research indicates dysregulation of these networks contributes to ADHD.
The PNRS didn't match polygenic risk scores, which indicate a person's genetic likelihood to have ADHD, suggesting environmental influences also contribute. Mooney and team conclude that more research is still needed to determine how genes, environment, and brain connections all interact to cause ADHD.
That said, PNRS could be a useful predictor of ADHD, and potentially reveal connections with other conditions like depression. By combining it with other factors, we might gain valuable insights into neurological behavioral disorders.
"The findings highlight the promise of approaches examining cumulative, brain-wide effects, and the importance of using large samples for improving reproducibility of neuroimaging studies," the authors write.
The study has been published in The Journal of Neuroscience.