A rare vomiting condition associated with chronic cannabis use is becoming more common at emergency departments in the US.
The condition, called cannabinoid hyperemesis syndrome (CHS), is marked by severe and cyclical bouts of uncontrollable nausea, abdominal pain, and vomiting.
The first case in the US was only reported in 2009, and until recently, CHS did not even have a national diagnostic code, making it a challenge to track.
Visits to the emergency room are one of the only ways to identify who is affected and why.
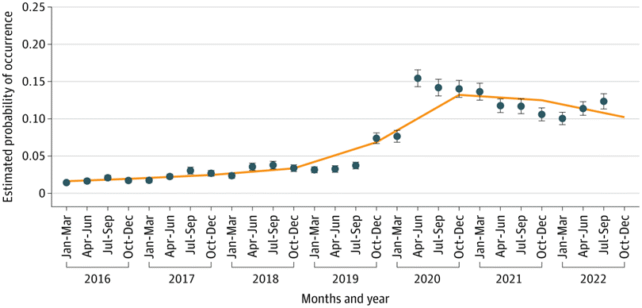
Between 2016 and 2022, researchers at the University of Illinois Chicago found that CHS visits to emergency departments rose from roughly 4 visits per 100,000 people visiting the emergency department to 22 visits per 100,000.
Related: Cannabis Use Is Linked to Epigenetic Changes, Scientists Discovered
While the findings suggest CHS is still rare, it's a trend to keep an eye on, especially when there is a way to stop the symptoms.
Just because someone uses cannabis or does so frequently does not mean they are doomed to develop CHS. No one knows why CHS affects a small proportion of cannabis users, but it is associated with frequent use, especially among those of younger ages.
The syndrome typically develops gradually over the first few years after initial use, with morning nausea or tummy pain, and can last for years.
The more severe stage arrives later, when, for a day or two after cannabis use, patients are beset by overwhelming and recurrent vomiting and nausea.
Strangely enough, a hot bath or shower can sometimes relieve these horrible symptoms, albeit temporarily.
Halting the use of cannabis can resolve the condition.
During the COVID-19 pandemic from 2020 to 2021, public health scientists James Swartz and Dana Franceschini found that CHS prevalence in US emergency departments increased significantly.
Their research analyzed roughly 806 million ER visits nationwide across the total period (2016-2022), and it is only the third national study to investigate CHS trends in US emergency departments.
Hospital visits for CHS were commonly made by people aged around 30, with slightly more female than male cases. The condition was most prominent in the West and Northeast compared with the South.
Whether or not that increase is due to more people using cannabis frequently or due to improved awareness is unknown.
Swartz and Franceschini argue that the COVID-19 pandemic likely catalyzed the recent rise in CHS through stress, isolation, and increased cannabis use.
Other researchers, however, point out that the increased percentage of diagnoses may not be due to increased cannabis use.
Rather, it could stem from increased recognition of CHS and a publication bias for a newly recognized syndrome.
In the past, researchers have described CHS as "rare but relevant" and often misunderstood. In certain published case studies, it's taken up to 17 hospital admissions to receive a diagnosis. Some patients are even accused of exaggerating their symptoms.
If someone presents to the hospital with symptoms of CHS, they must be diagnosed through exclusion, after ruling out all other possible explanations.
The condition has often been misdiagnosed as cyclical vomiting syndrome, which is treated differently. Cannabis use is key to whittling down the diagnosis, and yet that is a question some physicians don't think to ask, or some patients are unwilling to share answers to.
"The absence of a clear rise in CHS prior to 2020, despite expanding cannabis legalization and increasingly available high-potency products, presents a paradox," admit Swartz and Franceschini.
"One possibility is underdiagnosis or misclassification before the syndrome gained broader clinical recognition. The post-2020 surge may thus reflect both increased exposure as well as increased diagnostic vigilance."
Better diagnostics and further research are needed before researchers can truly say how rare CHS is.
The study was published in JAMA Network Open.

