'Mini-brains' grown in the lab allow scientists to study brain wiring without interfering with brains in living people, and now a new study has used these scaled-down models to identify neural signatures associated with schizophrenia and bipolar disorder.
Also known as organoids, the pea-sized brains are the work of a team led by researchers from Johns Hopkins University in the US. Further down the line, they could help pinpoint brain irregularities that might be targeted with treatments.
Both schizophrenia and bipolar disorder are currently diagnosed based on a person's clinical symptoms rather than biological markers. This new approach has the potential to provide a more objective and reliable method for identifying these psychiatric conditions.
Related: 14 Psychiatric Disorders Share 5 Genetic Roots, Major Study Reveals
"Schizophrenia and bipolar disorder are very hard to diagnose because no particular part of the brain goes off," says biomedical engineer Annie Kathuria, from Johns Hopkins University.
"No specific enzymes are going off like in Parkinson's, another neurological disease where doctors can diagnose and treat based on dopamine levels, even though it still doesn't have a proper cure."
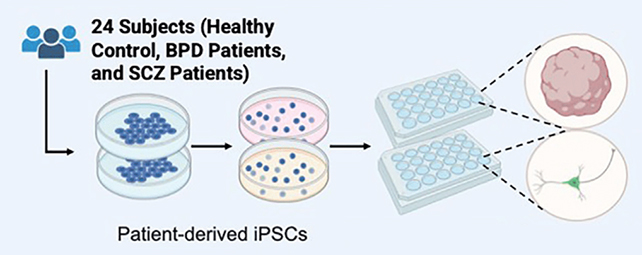
The brain organoids were engineered using blood and skin cells from people diagnosed with schizophrenia or bipolar disorder, and from people not diagnosed with any psychiatric conditions. That gave the researchers three categories of mini-brain to study.
Analyzed on a microchip and hooked up to a variety of sensors, the organoids are just 3 millimeters across (about a tenth of an inch), and were engineered to grow neural cell types from the brain's prefrontal cortex. This region plays a significant role in 'higher' cognitive functions, such as planning and decision-making.
With the help of machine-learning algorithms trained to detect patterns in neural communication, the team identified neuron activity unique to schizophrenia and bipolar disorder. These signatures were sufficient to correctly label the source of the cells in the organoids with 83 percent accuracy.
That accuracy rose to 92 percent when the mini-brains were given electrical stimulation, suggesting that the distinct neuron behavior is more pronounced – and easier to spot – when the brain is actively engaged and at work.
"At least molecularly, we can check what goes wrong when we are making these brains in a dish and distinguish between organoids from a healthy person, a schizophrenia patient, or a bipolar patient based on these electrophysiology signatures," says Kathuria.
As useful as these mini-brains are, they're still far less complex and nowhere near as functional as the real thing. So there's still plenty of work to be done here in terms of matching the patterns identified in this study with neural signatures in actual human brains.
Related: Scientists Pinpoint Where Extreme Moods of Bipolar Disorder Exist in the Brain
However, these are valuable indicators in understanding how the brains of people with schizophrenia or bipolar disorder might function differently. Every step forward in understanding how these conditions alter brain activity brings researchers closer to improved treatments.
"Our hope is that in the future we can not only confirm a patient is schizophrenic or bipolar from brain organoids, but that we can also start testing drugs on the organoids to find out what drug concentrations might help them get to a healthy state," says Kathuria.
The research has been published in APL Bioengineering.